-
Medical journals
- Career
POSTPARTUM SYMPHYSIOLYSIS - CASE STUDY SERIES - ANALYSIS OF LITERATURE AND OUR EXPERIENCE
Authors: Vojtěch Herrmann; Martin Křivohlávek; Jaroslav Šrám
Authors‘ workplace: Traumatologicko-ortopedické centrum, Krajská nemocnice Liberec, a. s.
Published in: Úraz chir. 28., 2021, č.1
Overview
In the presented case studies, the author summarizes his own experience with postpartum symphysiolysis. Based on this experience and a thorough analysis of the literature, the author subsequently outlines the possibilities of its diagnosis and treatment. Postpartum symphysiolysis is a rare injury that is only minimally mentioned in the literature. It is a multifactorial disease and due to the fact that it stands at the border of gynaecology, orthopaedics and traumatology, or anaesthesiology, it lacks clear and uniform recommendations in its diagnosis and treatment. In the last two decades, the number of published cases has increased significantly. This phenomenon may also be due to the fact that historically pelvic pain during pregnancy and childbirth was considered natural and not given much importance. Moreover, mild forms of diastasis often escape attention. The basic problem is the lack of systematic diagnostics on which subsequent recommendations can be based. An ultrasound examination of the pubic symphysis is a suitable method for diagnosis, ideally included in prenatal screening. The treatment is determined depending on the size of the symphyseal separation and the clinical difficulties of the patient. In mild forms, conservative therapy is the method of choice. In more severe forms, where both anterior and posterior pelvic injuries are combined, the choice of therapy remains controversial. One of the methods suitable for deciding on the therapeutic approach is skiascopic examination with pelvic residual stability test. If we proceed to the surgical solution, it turns out that all available methods show good results, whether it is external fixation, minimally invasive percutaneous fixation or open plate osteosynthesis.
OBJECTIVES OF THE WORK: Analysis of the literature and presentation of own experience.
TYPE OF WORK: Literature review, case studies.
MATERIAL: PubMED, ResearchGate, three case studies from our site from years 2010-2020.
METHODOLOGY: retrospective data collection, n=3.
Keywords:
Rare – pelvic injury – postpartum – symphysiolysis
INTRODUCTION
The pubic symphysis is a cartilaginous joint and its stability is ensured by a cartilaginous disc and four pubic ligaments (ligamentum pubicum superior, inferior, anterior, posterior). The disc and the anterior pubic ligament have the biggest influence on the stability [4]. During pregnancy, physiological changes take place in the pelvic ring in preparation for spontaneous labour. The symphysis is altered by the action of hormones such as estrogens, progesterone, but especially relaxin. It is produced by the placenta and from the first trimester of pregnancy onwards, it is responsible for the laxity of the ligaments and the natural diastasis of the pubic symphysis [31, 34]. The rapid advancement of the fetal head through the birth canal in the second stage of labour, its pressure on the bony pelvis and the short second stage of labour predispose possible rupture of the symphysis [33, 34]. Schoellner’s study on ultrasound measurements of symphysis width showed mean values of around 4 mm in non-pregnant women, 6.3 mm in asymptomatic symphysis diastasis and over 9.5 mm in symptomatic diastasis [28]. Values greater than 10 mm are generally considered pathological and carry clinical manifestations [11, 16, 21, 27].
Case study I.
A 31 years old woman (gravida 2, para 2) after spontaneous vertex birth complicated by dystocia. Immediately after delivery, she complained about severe pain above the pubic symphysis and the impossibility of verticalization. The attending physician indicated a pelvic X-ray with a finding of 30 mm symphysiolysis (Fig. 1). After a phone consultation, the patient was referred to our department. We added a CT scan of the pelvis, which showed enlargement of the left SI joint (Fig. 2). In the operating room, we first performed a stress test under skiascopic control with a finding of a 50 mm symphysiolysis. Pelvic ring instability was treated with an external fixator (Fig. 3). The ligamentous injury of the posterior pelvic segment was treated conservatively, without stabilization with an IS (iliosacral) screw. The postoperative course was uneventful with sitting and transfer to a wheelchair. Six weeks after surgery, we removed the external fixation and allowed the patient to walk with gradual weight-bearing. At the follow-up eight months after delivery, pain persisted in both SI joints. We performed a follow-up CT scan, which showed only minimal residual diastasis of the symphysis and the posterior segment of the pelvis was without pathological findings. The established regimen was continued, with the patient motivated to full exertion. At 10 months after the surgery, the patient was able to perform normal daily activities without difficulty, reporting only minimal low back pain after heavy exertion (Fig. 4).
Case study II.
Female 35 years old (gravida 6, para 4) after complicated induced spontaneous vertex birth. In the immediate aftermath of delivery, severe lower abdominal pain manifested, especially when walking. On the second day after delivery, the attending physician diagnosed intra-abdominal bleeding. A total of two surgical revisions of the bleeding in the Reitzus space were performed from the midline laparotomy. The patient was stabilized at the intensive care unit. Administration of a total of 13 erythrocyte transfusions was required. A 10 cm symphysiolysis was diagnosed on the fifth day after delivery and significant pelvic ring instability was treated with an external fixator. Our consult was requested and the patient was transported to our unit. Subsequently, conversion to internal osteosynthesis with a tension cerclage and plate was performed (Fig. 5). The postoperative course was uneventful with subsequent sitting and transfer to a wheelchair. After six weeks, the patient was allowed to walk. At the next follow-up, the patient reported persistent pain in both SI joints. We added a CT scan of the pelvis, which revealed the diastasis and vacuum phenomenon of the right SI joint. Seven months after delivery, the patient‘s difficulties persisted, stress incontinence was added, and a follow-up X-ray showed loosening of the osteosynthetic material (Fig. 6). We decided to remove it completely. However, this did not lead to an alleviation of the difficulties. We performed a follow-up CT scan of the pelvis, which showed regressive changes of the symphysis and sclerosis of the right SI joint. After mutual agreement with the patient, we did not indicate further surgery. The patient is dispensed on long-term at the urology and gynaecology department for persistent incontinence, dyspareunia and uterine prolapse. Even 10 years after the injury, lower back and symphysis pain persist during prolonged standing and after exertion.
Case study III.
A 21 years old woman (gravida 2, para 1) who had an induced delivery by spontaneous vertex birth after amniotomy. Subsequently, the gynaecologist treated a grade 2 perineal laceration suture. After delivery, the patient was unable to get out of bed. She reported severe pain above the pubic symphysis, a feeling of crepitation in the symphysis area on positioning. The traumatologist indicated an X-ray of the pelvis, which showed a 20 mm symphysiolysis. The patient was indicated for skiascopic examination under brief general anaesthesia in the operating theatre. This examination showed major laxity, symphysiolysis of 40 mm, and in addition a small avulsed bone fragment in the symphysis area. We opted for surgical therapy and performed repositioning and external fixation of the pelvis. The postoperative course was uneventful. The patient began rehabilitation, with sitting and transfers to a wheelchair. Six weeks after the surgery, the external fixator was extracted and walking was allowed. Three months after delivery, the patient was already walking with a full load. After ten months, she was without difficulty in normal daily activities, complaining only of minimal pain in both SI joints after prolonged exertion. Table 1 Summarizes the published case studies.
1. Summarizing the case studies published 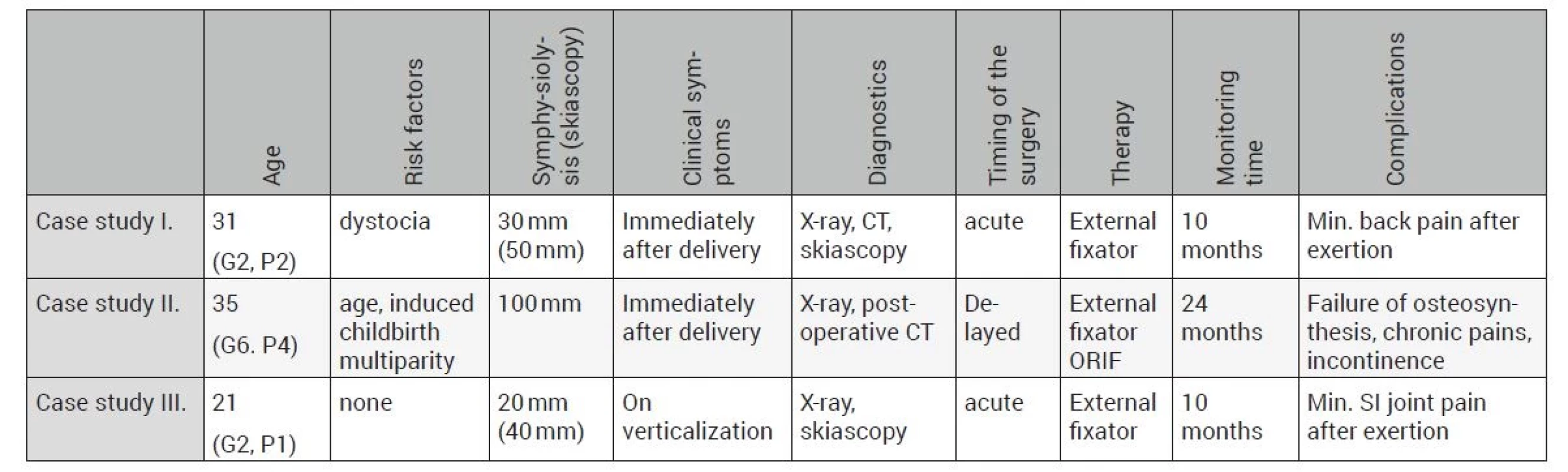
DISCUSSION
Symphysis and pelvic ring pain is a common phenomenon in the field of gynaecology and obstetrics. They are considered, like the diastasis of the symphysis, physiological. They often escape the attention of gynaecologists. The Leadbetter’s study even reported that pelvic pain accompanies 48–71% of pregnancies [19]. However, clinically significant symphyseal injury in the form of symphysiolysis after childbirth is very rare. The historical incidence rate is 1 : 300 to 1 : 30,000 births [8, 21, 24, 29]. It is very likely that in fact it will be closer to the former of the values. The underdiagnosis of this disease (especially in milder forms) is evident due to the fact that it is often underexamined by imaging methods and the treatment is mostly conservative in the sense of symptomatic pain management. More recent studies report an incidence of 1 : 569 and the most recent ones even 1 : 388 [29, 34].
The risk factors for the incidence of this injury are numerous. The most frequently mentioned are maternal age over 35 years, primiparity or multiparity, fetal macrosomia, cephalopelvic disproportion, forceps or vacuum extractor assisted delivery, precipitous delivery, dystocia, McRobertson’s manoeuver, hyperabduction of the parturient’s hips at delivery, epidural anaesthesia, dysplasia of the pregnant woman’s hips, or previous pelvic trauma [17, 21, 24, 27, 29, 33, 34]. Wang’s study described that elevated relaxin levels and birth weight correlate with a higher incidence of symphysiolysis but do not predict its severity [31]. Patients who have undergone symphysiolysis should be warned about the high rate of recurrence in subsequent pregnancies, in up to 68 – 85% of cases [16]. However, symphysiolysis at subsequent delivery is not associated with a worse outcome and should not be a barrier to future spontaneous delivery [26]. However, the decision on the form of labour management lies with the parturient and the attending gynaecologist.
The diagnosis is based on clinical findings followed by imaging. In the clinical picture, the typical symptoms are severe pain above the pubic symphysis and in the SI (sacroiliac) joint or LS (lumbosacral) spine, sometimes with projection to the lower limbs. Furthermore, inability to verticalize after the childbirth or severe pain when walking, especially up the stairs. Clinical tests include positive axial pressure on the hip blades, Trendelenburg sign or Faber (Patrick) test - painful hip flexion, abduction and external rotation [21, 33]. In some cases, symphysis rupture may even be accompanied by an audible clicking phenomenon [6].
X-ray examination in pregnancy is feared because of its possible negative impact on fetal development. Sonography thus appears to be sufficiently useful in the diagnosis of symphysiolysis. With ultrasound, the symphysis area is easily accessible and clear, and the symphysis diastasis can be easily measured [3]. This is confirmed by Iannell’s study on the extended FAST protocol (Focus assessment with sonography for trauma) in polytrauma or pelvic injuries with suspected pelvic ring injuries of the “open book” type. It reports a comparable yield compared to CT [15]. Thus, changes in the pubic symphysis can be evaluated by ultrasound repeatedly over time during pregnancy or as a one-time procedure when the patient has clinical difficulties. Magnetic resonance imaging could be used as a more detailed method, but it is not commonly available. X-ray and CT examinations find their dominant role particularly in the post partum period.
The literature shows that symphysis pubis diastasis above 10 mm is considered pathological [11, 16, 21, 27]. For values exceeding 25 mm, injury to the posterior segment of the pelvis must be considered. Most often in the form of ligamentous injury (ligamentum sacroiliacum anterior) with SI joint diastasis, in extreme cases also in the form of sacral fractures [20, 21, 32, 35]. Postpartum symphysiolysis is described in the classifications of pelvic fractures as type B1 - open book (Tile classification) or APC II (Young-Burgess classification).
A traumatologist or orthopaedic surgeon is informed about a serious postpartum pelvic injury only in the case of significant clinical difficulties. It should be kept in mind that severe pelvic ring injury during labour can be a source of massive haemorrhage and thus a lifethreatening condition requiring urgent surgical management [5]. The basic diagnostic examination methods include a plain radiograph of the pelvis, possibly supplemented by entrance and exit views. If a posterior pelvic segment injury is suspected, addition of a CT scan is appropriate. Kharazzi emphasizes the skiascopic examination of pelvic stability under general anaesthesia [17]. When diagnostic uncertainties arise, magnetic resonance imaging is preferably used [21, 27]. The decision on the therapeutic approach is still purely individual and empirical, depending on the patient’s current condition and the experience of the given site.
Treatment options range from conservative symptomatic therapy to open plate osteosynthesis of the symphysis and SI joint. Conservative therapy dominates the available literature, even with clinically significant findings, with good effect [6, 7, 12, 20, 25, 29, 30]. The gradual reduction of progesterone and relaxin hormone levels leads to the restoration of the original width of the symphysis within a few months after the birth (most often within 6 to 12 weeks). This is one of the arguments for choosing conservative therapy [26, 29, 33, 35]. Agten’s study based on magnetic resonance imaging provides information on changes in the symphysis during pregnancy and childbirth. Specifically, in STIR (short tau inversion recovery), three quarters of parturients show bone edema of the pubic symphysis after delivery (analogous to “bonebruise” in spinal injuries), regardless of whether the delivery was vaginal or caesarean. Thus, it shows changes in the signal intensity of the symphysis regardless of birth trauma [1].
In conservative therapy, pelvic girdle, lateral positioning, analgesics and physiotherapy with emphasis on strengthening the pelvic floor muscles are most commonly used [21, 30]. Intra-articular injections into the symphyseal joint with corticosteroids and local anaesthetic under ultrasound control have a great effect on the treatment of pain in the pre - and postnatal period. Even the administration of local anaesthetic alone parapubically without corticosteroids leads to a good effect [23]. Another option for analgesic therapy is the epidural anaesthesia. Supportive modalities may include electrostimulation or acupuncture [2, 9].
When the possibilities of conservative therapy are exhausted and in case of large clinical findings, surgical therapy is resorted to. However, the indication criteria for surgical therapy are a cause of controversy. In earlier studies, a symphyseal diastasis of 25 mm or more was reported as a decisive value, associated with a probable posterior pelvic segment injury [22]. On the other hand, cases with much larger findings managed conservatively with good outcome have been presented [7]. Kharazzi later updated the value of symphysiolysis indicating surgical therapy to 40 mm [17]. This value is now generally accepted by the majority [21, 32]. Another indication for postponed surgical treatment of postpartum symphysiolysis are the signs of chronic instability of the pelvic ring. Hagen defined four basic criteria for instability - symphysis diastasis greater than 1 cm, vertical shift greater than 0.5 cm, diastasis and paraarticular sclerosis at the SI joint [11].
The surgical solution consists of open repositioning and fixation with tension cerclage, screws and plates [21, 24, 33, 35] or treatment with an external fixator [8, 13]. The main advantage of surgical therapy is the prevention of chronic pelvic instability compared to conservative treatment. The general trend in surgical therapy is a minimally invasive osteosynthesis with percutaneously inserted screw(s) through the symphysis or with the TightRope implant [10]. The mechanical stability of each type of osteosynthesis and their long-term functional and graphic outcome remains a question. A cadaveric study demonstrated comparable stability results using the TightRope method and a single-plane six-hole plate. A comparison of a percutaneously inserted screw and a single-plane plate yielded similar results [14, 18]. It should be mentioned that symphysis osteosynthesis is accompanied by a high rate of implant failure at longterm follow-up (up to 43 % of cases); however, this failure is clinically asymptomatic in the vast majority of cases [21]. As mentioned above, as with other pelvic injuries, posterior segment involvement must be considered. For SI joint injuries or sacral fractures, percutaneous osteosynthesis with a cannulated screw is the gold standard treatment [24].
When deciding on the treatment of postpartum symphysiolysis, it is important to assess the possible complications associated with both surgical and conservative treatment. On the one hand, take into account the physiology and pathophysiology of the pregnancy and childbirth, especially the risk of bleeding complications. On the other hand, prolonged immobilization after birth trauma is associated with a higher risk of thromboembolic complications [2]. Another attribute associated with pregnancy is the reduced immunity of the pregnant woman, which is completely restored three to four months after delivery [21]. This fact can influence us when choosing between open and minimally invasive surgery.
Between 2010 and 2020, we treated surgically three cases of postpartum symphysiolysis. In one case, there was a dramatic finding of a 10 cm of symphysiolysis and massive gynaecological bleeding. Symphysiolysis was diagnosed and managed late, at five days after delivery, with an external fixator, with subsequent conversion to open osteosynthesis with tension cerclage and plate. In the other two cases, we used the external fixator as a definitive treatment. We emphasize the clinical examination of the patient, not just the evaluation of radiological findings. Except for the first case, we first examined the stability of the pelvic ring skiascopically. Both of these examinations showed more pronounced laxity in the symphysis area than was documented on standard radiographs. Following this, we proceeded to the surgical solution. The decision on the type of surgical therapy was purely empirical. The published set and retrospective follow-up are of course of little value, so we would like to address this issue in the future in closer cooperation with gynaecological departments in our region and particularly with traumatology and orthopaedic departments across the Czech Republic. This could yield an already larger patient pool with greater impact.
Following the analysis of the literature, it presents to propose a method of diagnosis, classification and subsequent choice of therapy of the symphysis injury during pregnancy and childbirth. Ultrasound measurements of the symphysis as a part of prenatal screening checks by the attending gynaecologist would be the basis for diagnosis. This would create a new screening “marker” in the pregnancy certificate. Potentially high-risk parturients with symptomatic diastasis of the symphysis would be selected. A routine X-ray examination of the pelvis after delivery could be a possible component. Pubic symphysis injury could be uniformly classified into three grades: 1) <25 mm, 2) 25–40 mm, 3)> 40 mm. Based on this classification, then determine the choice of therapy: 1st stage conservatively, 2nd stage “grey” zone (individual choice of the specialist, surgeon, skiascopy?), 3rd stage surgical solution.
CONCLUSION
Postpartum symphysiolysis does not have clear recommendations in documentation, diagnosis and treatment yet. Historically reported incidence rates are significantly underestimated. The clinical findings are typically severe pain above the pubic symphysis and difficult verticalization. Diagnosis is based on ultrasound in the antenatal period and on X-ray and CT scans after birth. Conservative therapy is the method of choice. In case of its failure or in case of clinically significant findings, the treatment is surgical. Symphysis diastasis greater than 40 mm is the threshold. The current trend is minimally invasive osteosynthesis. Other factors such as physiological and pathophysiological processes during pregnancy and childbirth must also be considered in the decision-making process of therapy selection. Also the personal experience of the given site and, last but not least, the psychological impact on the new mother, her and her child‘s needs and the shortest possible recovery. Based on our own experience, symphysiolysis must first of all be thought of as a possible postpartum injury. Its delayed diagnosis can have fatal consequences. Close interdisciplinary cooperation is important. Even nowadays we take clinical examination as an irreducible basis. Radiodiagnosis is based on a radiograph of the pelvis. A CT scan is necessary to complete the diagnosis. Skiascopic examination of pelvic ring instability is considered to be very helpful in deciding on the method of therapy. It seems that acute management of symphysiolysis with an external fixator is also suitable as a definitive treatment, yielding good results in combination with minimally invasive surgery and minimal time.
Sources
1. AGTEN, CA, METZLER, C., ROSSKOPF, AB. et al. MR imaging of pubic symphysis after uncomplicated vaginal delivery and planned caesarean delivery in the first postpartum week. Clinical imaging. 2019, 56, 58–62. https://doi.org/10.1016/j.clinimag.2019.03.009.
2. AYENI, G., OLADIRE, O., JOVITA, D. et al. Transcutaneous Electrical Nerve Stimulation (TENS) in the Management of Peripartum Diastasis Symphysis Pubis (DSP): Cases Report. Indian Journal of Physiotherapy and Occupational Therapy - An International Journal, 2015. https://doi.org/10.5958/0973-5674.2014.00001.X.
3. BECKER, I., STRINGER, MD, JEFFERY, R. et al. Sonographic anatomy of the pubic symphysis in healthy nulliparous women. Clinical anatomy (New York, N.Y.), 2014, 27, 7, 1058–1067. https://doi. org/10.1002/ca.22423.
4. BECKER, I., WOODLEY, SJ, STRINGER, MD. The adult human pubic symphysis: a systematic review. Journal of anatomy, 2010, 217, 5, 475–487. https://doi.org/10.1111/j.1469-7580.2010.01300.x. 5. BUITENDYK, M., BRENNAN, B., VORA, P. et al. Acute Intrapartum Rupture of the Pubic Symphysis Requiring Resuscitation and Surgical Intervention: A Case Report. JOGC, 2018, 40, 1, 68–71. https://doi.org/10.1016/j.jogc.2017.05.028
6. COWLING, PD, RANGAN, A. A case of postpartum pubic symphysis diastasis. Injury. 2010, 41, 6, 657–659. https://doi.org/10.1016/j. injury.2010.01.112.
7. DEEPENDRA, S., MAYANK, V., AKHIL, B. et al. Post Partum Pubic Symphysis Disruption Following Normal Full Term Vaginal Delivery: A Rare Case Report. NJMDR, 2015, 3, 56-59.
8. DUNIVAN, GC, HICKMAN, AM, CONNOLLY, A. Severe separation of the pubic symphysis and prompt orthopedic surgical intervention. Obstetrics and gynecology. 2009, 114, 2, 473–475. https://doi. org/10.1097/AOG.0b013e3181998bd1.
9. ELDEN, H., LADFORS, L., OLSEN, MF. et al. Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. BMJ, 2005, 330, 7494, 761. https://doi.org/10.1136/ bmj.38397.507014.E0.
10. FENG, Y., HONG, J., GUO, X. et al. Percutaneous fixation of traumatic pubic symphysis diastasis using a TightRope and external fixator versus using a cannulated screw. Journal of orthopaedic surgery and research, 2016, 11, 1, 62. https://doi.org/10.1186/s13018 - 016-0397-7.
11. HAGEN, R. Pelvic girdle relaxation from an orthopaedic point of view. Acta orthopaedica Scandinavica. 1974, 45, 4, 550–563. https://doi.org/10.3109/17453677408989178.
12. HERREN, C., SOBOTTKE, R., DADGAR, A. et al. Peripartum pubic symphysis separation-Current strategies in diagnosis and therapy and presentation of two cases. Injury. 2015, 46, 6, 1074–1080. https://doi.org/10.1016/j.injury.2015.02.030.
13. CHANG, JL, WU, V. External fixation of pubic symphysis diastasis from postpartum trauma. Orthopedics. 2008, 31, 5, 493. https:// doi.org/10.3928/01477447-20080501-05.
14. CHEN, L., ZHANG, G., SONG, D. et al. A comparison of percutaneous reduction and screw fixation versus open reduction and plate fixation of traumatic symphysis pubis diastasis. Archives of orthopaedic and trauma surgery, 2012, 132, 2, 265–270. https://doi. org/10.1007/s00402-011-1414-2.
15. IANNIELLO, S., CONTE, P., DI SERAFINO, M. et al. Diagnostic accuracy of pubic symphysis ultrasound in the detection of unstable pelvis in polytrauma patients during e-FAST: the value of FASTPLUS protocol. A preliminary experience. Journal of ultrasound. 2020, 10.1007/s40477-020-00483-6. Advance online publication. https://doi.org/10.1007/s40477-020-00483-6.
16. JAIN, S., EEDARAPALLI, P., JAMJUTE, P. et al. Symphysis pubis dysfunction: a practical approach to management. The Obstetrician & Gynaecologist. 2006, 8 : 153-158. https://doi.org/10.1576/ toag.8.3.153.27250
17. KHARRAZI, FD, RODGERS, WB, KENNEDY, JG et al. Parturition - induced pelvic dislocation: a report of four cases. Journal of orthopaedic trauma. 1997, 11, 4, 277–282. https://doi. org/10.1097/00005131-199705000-00009.
18. KISKADDON, EM, WRIGHT, A., MEEKS, BD et al. A biomechanical cadaver comparison of suture button fixation to plate fixation for pubic symphysis diastasis. Injury. 2018, 49, 11, 1993–1998. https://doi.org/10.1016/j.injury.2018.09.032.
19. LEADBETTER, RE, MAWER, D., LINDOW, SW. Symphysis pubis dysfunction: a review of the literature. The journal of maternalfetal & neonatal medicine. 2004, 16, 6, 349–354. https://doi. org/10.1080/14767050400018247.
20. NITSCHE, JF, HOWELL, T. Peripartum pubic symphysis separation: a case report and review of the literature. Obstetrical & gynecological survey. 2011, 66, 3, 153–158. https://doi.org/10.1097/ OGX.0b013e31821f84d9.
21. NORVILAITE, K., KEZEVICIUTE, M., RAMASAUSKAITE, D. et al. Postpartum pubic symphysis diastasis-conservative and surgical treatment methods, incidence of complications: Two case reports and a review of the literature. World journal of clinical cases. 2020, 8, 1, 110–119. https://doi.org/10.12998/wjcc.v8.i1.110.
22. PAUWELS, F. Beitrag zur Klärung der Beanspruchung des Beckens, insbesondere der Beckenfugen. Gesammelte Abhandlungen zur funktionellen Anatomie des Bewegungsapparates. Springer, Berlin, Heidelberg. 1965. https://doi.org/10.1007/978-3-642-86841-2_3.
23. POMP, G. Symphysiolysis and Pregnancy Related Pelvic Girdle Pain – Mystery Resolved?, WCGO 2020, 3rd world congress on Gynecology and obstetrics,Webinar, August 31st -September 01st, 2020, ISSN:2591-7994.
24. ROMMENS, PM. Internal fixation in postpartum symphysis pubis rupture: report of three cases. Journal of orthopaedic trauma. 1997, 11, 4, 273–276. https://doi.org/10.1097/00005131-199705000 - 00008.
25. SEIDMAN, A., BROSSY, K., FAULKNER, A. et al. Traumatic Pelvic Ring Injury following Childbirth with Complete Pubic Symphysis Diastasis. Case reports in orthopedics, 2019, 1785167. https://doi. org/10.1155/2019/1785167.
26. SENECHAL, PK. Symphysis pubis separation during childbirth. The Journal of the American Board of Family Practice. 1994, 7, 2, 141–144.
27. SHNAEKEL, KL, MAGANN, EF, AHMADI, S. Pubic Symphysis Rupture and Separation During Pregnancy. Obstetrical & gynecological survey. 2015, 70, 11, 713–718. https://doi.org/10.1097/ OGX.0000000000000247.
28. SCHOELLNER, C., SZÖKE, N., SIEGBURG, K. Der schwangerschaftsassoziierte Symphysenschaden aus orthopädischer Sicht-Untersuchungen zu Veränderungen an der Symphysis pubica in der Schwangerschaft, unter der Geburt und post partum. Zeitschrift fur Orthopadie und ihre Grenzgebiete. 2001, 139, 5, 458–462. https:// doi.org/10.1055/s-2001-17991.
29. SNOW, RE, NEUBERT, AG. Peripartum pubic symphysis separation: a case series and review of the literature. Obstetrical & gynecological survey. 1997, 52, 7, 438–443. https://doi.org/10.1097/00006254 - 199707000-00023.
30. URRACA-GESTO, MA, PLAZA-MANZANO, G., FERRAGUT-GARCÍAS, A. et al. Diastasis of symphysis pubis and labor: Systematic review. Journal of rehabilitation research and development. 2015, 52, 6, 629–640. https://doi.org/10.1682/JRRD.2014.12.0302.
31. WANG, Y., LI, YQ, TIAN, MR et al. Role of relaxin in diastasis of the pubic symphysis peripartum. World journal of clinical cases. 2021, 9, 1, 91–101. https://doi.org/10.12998/wjcc.v9.i1.91.
32. WANG, Y., WU, XB, YANG, MH. et al. Beijing da xue xue bao. Yi xue ban. Journal of Peking University. Health sciences. 2015, 47, 2, 368–372.
33. WENDSCHE, P., VESELÝ, R., KEPÁK, P. et al. Úskalí a komplikace při léčení zlomenin. Praha: Galén, 2018. 483 s. ISBN 978-80-7492-393 - 7.
34. YOO, JJ, HA, YC, LEE, YK et al. Incidence and risk factors of symptomatic peripartum diastasis of pubic symphysis. Journal of Korean medical science. 2014, 29(2), 281–286. https://doi.org/10.3346/ jkms.2014.29.2.281.
35. HOU, Z., RIEHL, JT, SMITH, WR et al. Severe postpartum disruption of the pelvic ring: report of two cases and review of the literature. Patient Saf Surg. 2011, 5, 2. https://doi.org/10.1186/1754 - 9493-5-2.
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2021 Issue 1-
All articles in this issue
- IN MEMORIAM prof. MUDr. Libor Paša, PhD.
- IN MEMORIAM MUDr. Pavel Kopačka
- IN MEMORIAM prof. MUDr. Miroslav Zeman, DrSc.
- OSTEOSYNTHESIS OF HUMERAL DIAPHYSEAL FRACTURE BY INTRAMEDULLARY NAIL WITH ELECTROMAGNETIC DISTAL LOCKING - INTRODUCTION OF THE METHOD AND FIRST EXPERIENCE
- C-NAIL – 8-YEAR TREATMENT RESULTS
- POSTPARTUM SYMPHYSIOLYSIS - CASE STUDY SERIES - ANALYSIS OF LITERATURE AND OUR EXPERIENCE
- OSTEOSYNTHESIS OF THE POSTERIOR PELVIC SEGMENT WITH ILIOSACRAL SCREWS UNDER 3D NAVIGATION CONTROL
- Trauma Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- POSTPARTUM SYMPHYSIOLYSIS - CASE STUDY SERIES - ANALYSIS OF LITERATURE AND OUR EXPERIENCE
- OSTEOSYNTHESIS OF HUMERAL DIAPHYSEAL FRACTURE BY INTRAMEDULLARY NAIL WITH ELECTROMAGNETIC DISTAL LOCKING - INTRODUCTION OF THE METHOD AND FIRST EXPERIENCE
- IN MEMORIAM prof. MUDr. Libor Paša, PhD.
- OSTEOSYNTHESIS OF THE POSTERIOR PELVIC SEGMENT WITH ILIOSACRAL SCREWS UNDER 3D NAVIGATION CONTROL
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career







