-
Medical journals
- Career
Abdominal compartment syndrome in polytrauma
Authors: Jan Stránský; Milan Šír; Leopold Pleva
Authors‘ workplace: Lékařská fakulta Ostravské univerzity ; Traumatologické centrum Fakultní nemocnice Ostrava
Published in: Úraz chir. 25., 2017, č.4
Overview
INTRODUCTION:
Abdominal compartment syndrome is a serious and potentially life-threatening complication, which occurs in patients with serious abdominal trauma. It originates as a consequence of elevation in intraabdominal pressure, and the related effects imposed upon ventilation and circulation, including microcirculation. The condition is manifested with hypoventilation, negative impact upon the heart function and organ dysfunction. In order to diagnose the syndrome, we most frequently use the measurement of intravesical pressure, together with evaluation of the patient’s clinical condition.
MATERIAL:
The authors report on a group of 15 patients with a developed abdominal compartment syndrome hospitalized at the Trauma Centre, University Hospital Ostrava between 2006 and 2015. These patients represent a subgroup from 422 patients, who underwent a surgical procedure due to abdominal trauma at our centre during that time.
RESULTS:
From the group of 15 patients with a developed abdominal compartment syndrome, 6 patients died. All patients sustained a serious polytrauma. Decompression surgery was performed in 2 patients immediately after admission to the hospital, in the remaining patients, the procedure was performed after 2.81 days on average. In the following text, the authors present a detailed analysis of the development of the condition in selected cases.
CONCLUSION:
We consider the values of intra-abdominal pressure exceeding 20 mmHg, with a simultaneous presence of clinical manifestations, to be an indication for performing a decompressive laparostomy. This procedure may be also performed preventively, in patients with serious abdominal trauma, in whom it is possible to anticipate further development of abdominal compartment syndrome, already according to the initial findings.
KEYWORDS:
Abdominal compartment syndrome, abdominal trauma, intra-abdominal pressure, laparostomy.
INTRODUCTION
Compartment syndrome is generally described as a condition, when pressure increases in a bordered anatomical space, which adversely affects the circulation, and endangers the functionality and vitality of tissues or organs in this space. This condition may develop in osteofascial spaces of extremities, intracranially, or in the chest and abdominal cavity [7].
Abdominal compartment syndrome (ACS) is defined as a late manifestation of increased intraabdominal pressure (IAP). This condition is associated with a significant morbidity and mortality [8]. A number of reports dealing with this problem have been published in the recent years, on the basis of which the World Society of the Abdominal Compartment Syndrome (WSACS) developed consensual definitions of terms and recommendations for the treatment of ACS.
In trauma patients, increased IAP, and possible subsequently developed ACS, are most frequently observed in patients with a serious abdominal trauma, either primarily or secondarily [18].
Causes of primary ACS development:
- Massive intra-abdominal and retroperitoneal haemorrhage.
- Bleeding due to development of posttraumatic coagulopathy.
- Distension and oedema of intestinal loops due to an injury of mesenteric vessels.
- Accumulation of coagula, or tamponade of non-surgical haemorrhage in the subphrenic, pelvic or retroperitoneal space.
- Perforating injury of the GIT, with subsequent development of peritonitis and ileus.
Causes of secondary ACS development:
- Resuscitation with excessive use of crystaloids.
- Abdominal wall closure under tension.
Typical clinical manifestations of a developed ACS:
- Abdominal wall distension (Fig. 4).
- Respiratory insufficiency, associated with an increase of inspiration pressures due to elevated diaphragm, hypoxia and hypercapnia.
- Decreased cardiac performance.
- Oliguria or anuria with preserved MAP.
PATIENTS
A total of 422 abdominal surgeries were performed at the Trauma Centre of the University Hospital Ostrava between 2006 and 2015 (tab. 1). Large numbers of these injuries were a part of more extensive polytraumas. Considering the aetiology of injuries, traffic accidents and falls from height prevailed (tab. 2). Another significant group were work-related injuries, such as being crushed with a work machine and burials under earthfalls or loads. The group of crime-related injuries, such as stab wounds or gunshot wounds, was more frequently represented as isolated injuries, or compound injuries, with a less serious impairment of other body regions.
1. Complete overview of observed injuries 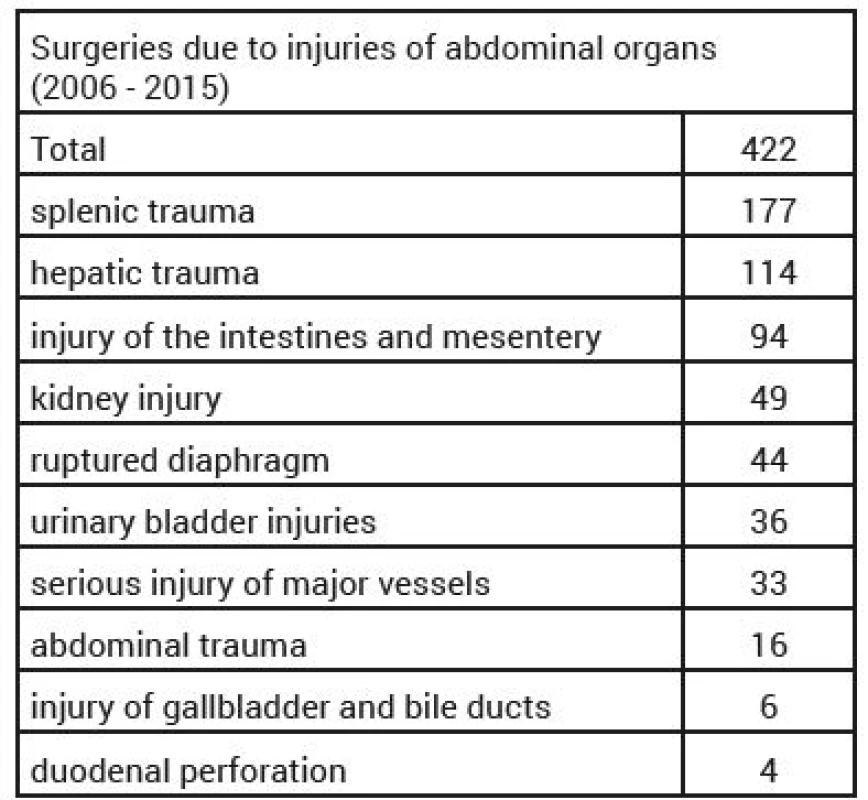
2. Causes of trauma in patients with ACS 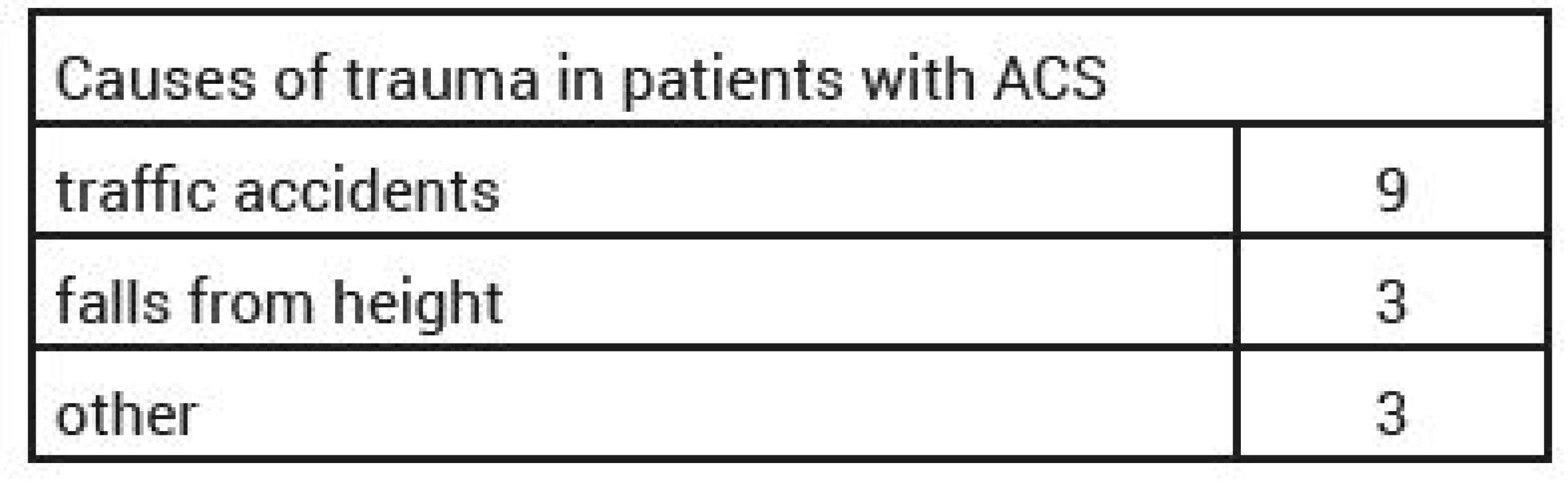
We observed a total of 15 cases of ACS development among our patients, there were 9 men and 6 women. The age spectrum was from 10 to 69 years (average 43.4, median 43). The patients predominantly sustained a serious polytrauma, with ISS of 27–66 (average 39.8, median 38); in one case, the patient suffered an isolated abdominal injury after being kicked by a horse, with liver laceration. The dominating cause of injury was traffic-related injuries (8 in total). Furthermore, we noted 3 cases of falls from heights, 1 case of brachial violence among partners, 1 case of burial under a tree trunk during felling of trees, and 1 case of suicidal attempt by jumping in front of a train.
A serious abdominal injury was present in 14 cases (tab. 3). An associated chest trauma was present in 11 patients (multiple rib fractures, lung injury), significant limb trauma in 5 patients; we also observed three cases with pelvic fractures. In two cases, trauma of the abdominal aorta was diagnosed; one of the cases was treated with suture, the other one with stent placement. One female patients sustained a serious concomitant cranial trauma, which resulted in the patient’s death on the 6th day after trauma.
3. Division of intraabdominal hypertension (IAH) according to WSACS 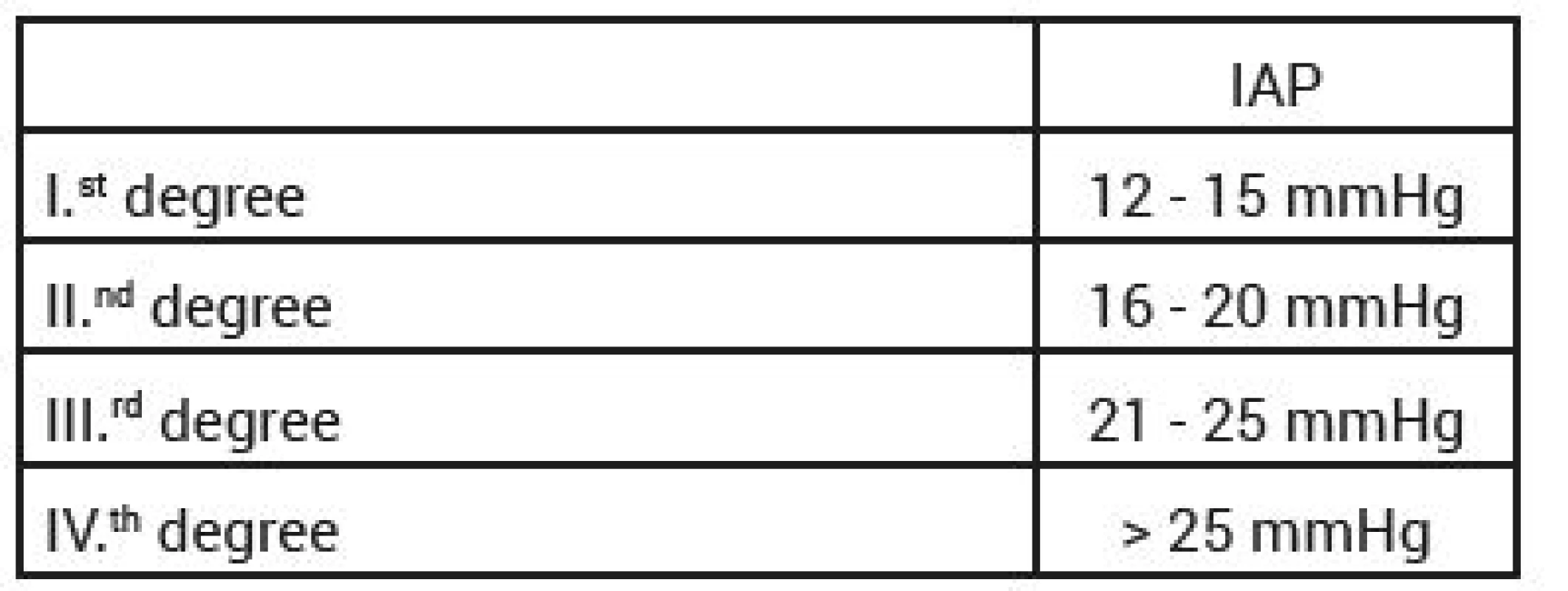
RESULTS
A total of 6 patients died from our patient file. Four deaths were due to MODS and MOF development within 24 hours to 30 days from the injury. One death was caused by the already mentioned cranial trauma, and the last death was caused by irreversible traumatic-haemorrhagic shock in the patient with suicidal attempt by jumping in front of a train. This patient was admitted in a critical condition, and required an emergency completion of trauma amputations of both lower limbs and the right upper extremity; subsequently performed CT examination showed a minimum of free fluid in the abdominal cavity. However, after 21 hours from the injury, due to generally worsening medical condition of the patient, and the clinical findings in the abdominal cavity, laparotomy was performed with a finding of minor ruptures of the mesentery, caecum and ileum, with extensive surrounding contusions. These were treated with sutures and laparostomy, however, the patient died after 5 more hours.
In two patients, decompression of the abdominal cavity was performed immediately upon admission. Both patients were admitted 12–15 hours after the initial trauma. A 38-year old woman was beaten by her partner at home, found unconscious, transferred to emergency room already intubated, hypotensive, on vasopressors. Clinical examination revealed distension of the abdominal wall, absence of peristalsis, numerous haematoma. CT examination showed hemopneumoperitoneum, with suspected duodenal injury and kidney contusion. Revision of the abdominal cavity was performed, with a finding of almost complete duodenal rupture in the D2 segment, and extensive mesocolon necroses. Hemicolectomy was performed, followed by a resection of the duodenum, with its dead end occlusion. The abdominal cavity was left open. Nevertheless, the patient died after 16 hours due to a developed septic shock. The second case was a 36-year old man, pedestrian hit by car. The patient was initially admitted to an Anaesthesiology and Resuscitation Department of a regional hospital. Initially restless, intubated. Radiographs revealed a 2-cm symphyseolysis and acetabular fracture on the left. Ultrasound examination showed no free fluid in the abdominal cavity, cerebral CT could not be evaluated; furthermore, the patient sustained fracture of the crus and multiple soft tissue contusions. Pelvic clamp was used at the operating theatre, due to the developing circulatory instability and fear of pelvic haemorrhage, with explorative laparotomy, without any findings of a more significant source of bleeding, with a complete closure of the abdominal cavity. A total of 7.5 litres of fluids was administered during resuscitation, 26 TU EBR and 22 TU FFP, Novoseven, Fibrinogen, platelet concentrates. The patient was transported by air ambulance to the Trauma Centre of the University Hospital Ostrava approximately 12 hours after the injury. The patient was intubated upon admission, with distended abdomen (Fig. 1), no audible peristalsis, cold peripheral areas with weary capillarity, anuric. On CT, subarachnoid haemorrhage (SAH) T-O bill., minor contusions F-P on the right, P on the left, fracture of nasal bones, bleeding into paranasal cavities, fluidothorax bill., dosrobasal pulmonary contusion, air bubbles in portal circulation, borders of fluid below the liver, spleen and around the pancreas, also around psoas on the left, interclavicular haematoma, significant distension of intestinal loops, intestinal paralysis, air in the intestinal wall and the mesenteric venous system and upper mesenteric vein (Fig. 2), fractures of Th11 and Th12, fracture of the lower arm of pubic symphysis on the right, anterior acetabular column on the right, symphysiolysis. Exploration of the abdominal cavity was performed immediately, with the findings of minimal hemoperitoneum, extensive gangrene of the loops of small intestine (Fig. 3) and the ascendant, sterocoral peritonitis, and a massive retroperitoneal haematoma. Resection of loops of the small intestine and hemicolectomy were performed (Fig. 4), with laparostomy and stabilization of the pelvis using external fixator. Despite the subsequent resuscitation care, the patient died 24 hours later.
1. Clinical picture of ACS – abdominal wall distension 
2. CT findings of developed ACS – interclavicular haematoma, significant distension of the loops, image of intestinal paralysis, air in the abdominal wall and the vascular system of the mesentery 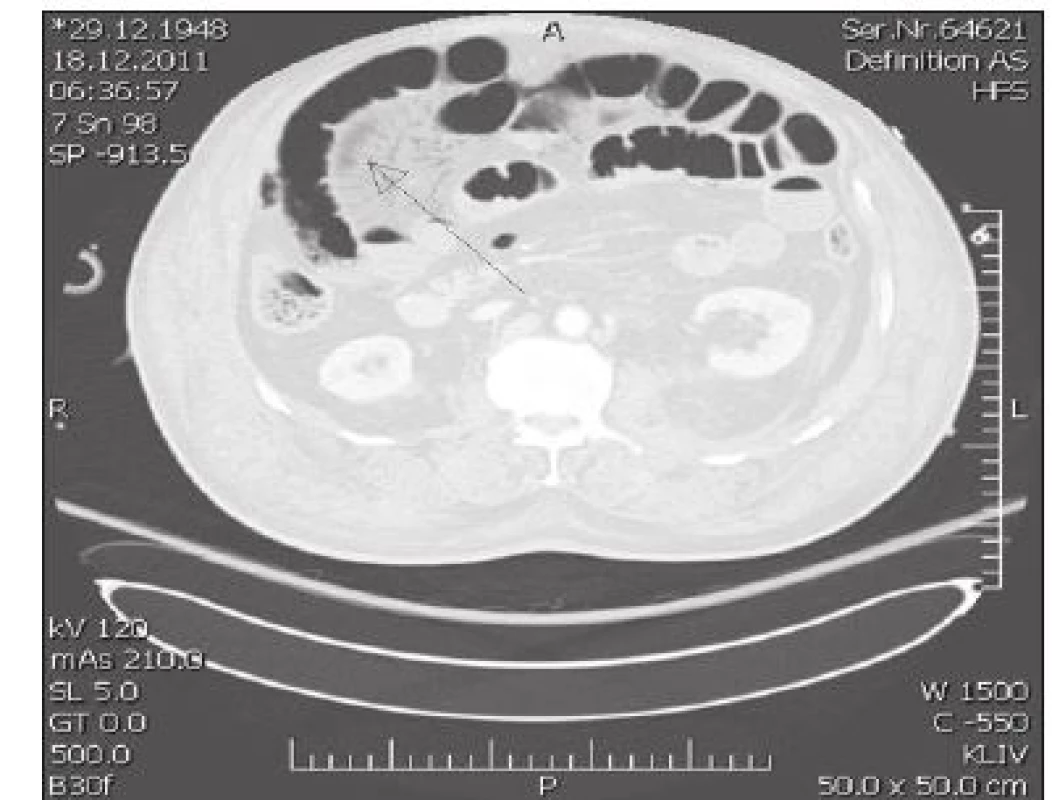
3. Necrosis of a loop of small bowel in a patient with developed ACS 
4. Resected loop of small bowel and caecum 
In the other patients, decompression surgery was performed on average 2.81 days after injury (median 2). Laparostomy was performed in all cases, with a temporary closure of the abdominal cavity using hydrophobic drapes, Ethizip, or the VAC. system (Fig. 5).
5. Laparostomy using the VAC system 
Definite closure of the abdominal cavity followed after 3 days at the earliest, and 10 days at the latest. In one case, the open-abdomen was left in place for the period of 30 days in a patient with aortic dissection, in whom repeated revisions of the abdomen and retroperitoneum were required. The patient’s condition further deteriorated, and resulted in the patient dying 30 days from the injury due to MOF and MODS. We observed the incidence of ACS at 3.6 %, which corresponds with the values reported in world literature for patients with abdominal trauma.
DISCUSSION
ACS is associated with serious abdominal and systemic consequences [11]. The mortality rate in fulminant ACS reaches up to 67 % [1]. Except for the already mentioned clinical introduction, the increase of IAP and ACS development have also other pathophysical relations. In the circulatory system, it is namely a decrease of the cardiac output, decreased venous return and increase of peripheral vascular resistance. Experimental works have shown that elevated IAP is the cause of impaired intestinal perfusion, leading to an increased production of oxygen free radicals and bacterial translocation through the intestinal wall [6]. Another experimental work demonstrates that increase of IAP above the value of 25 mmHg for the period of 60 minutes leads to a decrease of the partial oxygen pressure in the intestinal mucosa to less than 30 % [3]. Elevated IAP is also the cause of alteration of hepatic functions, with deepening of the metabolic acidosis and coagulopathy, which, in a circle, further supports the increase of IAP. Due to the fact that ACS development presents a serious threat for patients with polytrauma, often with associated craniocerebral trauma, it is not possible to omit the relation between elevated IAP and the increase of intracranial pressure (ICP), with a related decrease of the cerebral perfusion pressure and a risk of ischemic damage [2].
In order to be able to sense the danger associated with increasing IAP, and implement a timely prevention of ACS development, it is necessary to monitor the IAP in high-risk patients. The most frequently used technique for this purpose is intravesical measurement, which is a simple and reliable technique, which is also minimally invasive. The basic principles of this technique were described in 1984 by Kron et al. The measurement is performed by administering 50–100 ml of saline into the urinary bladder, via Foley catheter. A clamp is placed on the catheter, and a converter system with manometer is attached [14]. Significant differences in IAP measurement were demonstrated, depending on the position of the pressure converter (at the level of symphysis or flebostatic axis). In order to obtain comparable measurements, it is recommended to use the middle axial line as a referential level in a lying patient [4]. At present, there are many commercially available sets intended for this measurement. Based upon these values, WSACS defines four degrees of intraabdominal hypertension (IAH) (Tab. 3). Surgical decompression is indicated in 3rd and 4th degree [17].
WSACS defines ACS as IAP>20 mmHg, refractory to conservative procedures, with manifestations of organ failure [15]. In these cases, surgical decompression of the abdominal cavity is clearly indicated. In patients with the presence of two and more risk factors for IAH/ACS, monitoring of IAP should be performed for the whole period when the patient is in a critical condition, in the interval of at least 4 hours [10]. These high-risk patients require a use of available conservative means in the attempt to normalize IAP and prevent the development of ACS. These procedures include evacuation of the GIT contents, with insertion of a gastric tube and rectal tube, in order to support the passage of prokinetics. Decreasing the volume of enteral feeding, or possibly switching to purely parenteral nutrition is recommended. Analgetization should be administered, together with appropriate sedation and muscle relaxation, with a continuous evaluation of their possible negative effects. It is also important to maintain fluid balance, with limitation of excessive fluid resuscitation, which may be supported with diuretics, by administration of hyperosmolar solutions and coloids. Furthermore, it is also important to maintain the abdominal perfusion pressure (APP) above 60 mmHg by administration of vasopressors [9]. Attention should be paid to the position of the body, with elimination of the prone position, and prevention of elevation of the upper part of the body by more than 20° against the bed, which significantly increases IAP [16]. Surgical treatment means decompression surgery. During the surgical procedure, blood is removed from the abdominal cavity, together with all coagula and other secretions. All possible sources of bleeding should be carefully examined and treated (ligatures, local injection). Persisting non-surgical bleeding may be treated with tamponade. The abdominal cavity is washed out with a warm saline [18]. The abdomen is left open. In order to close the laparotomy, a number of techniques may be used. Hydrophobic foils, Ethizip, Bogota bag, vaccum-assisted closure (VAC), and others (Fig. 6, 7).
6. Treatment of ACT – decompression, hydrophobic drapes 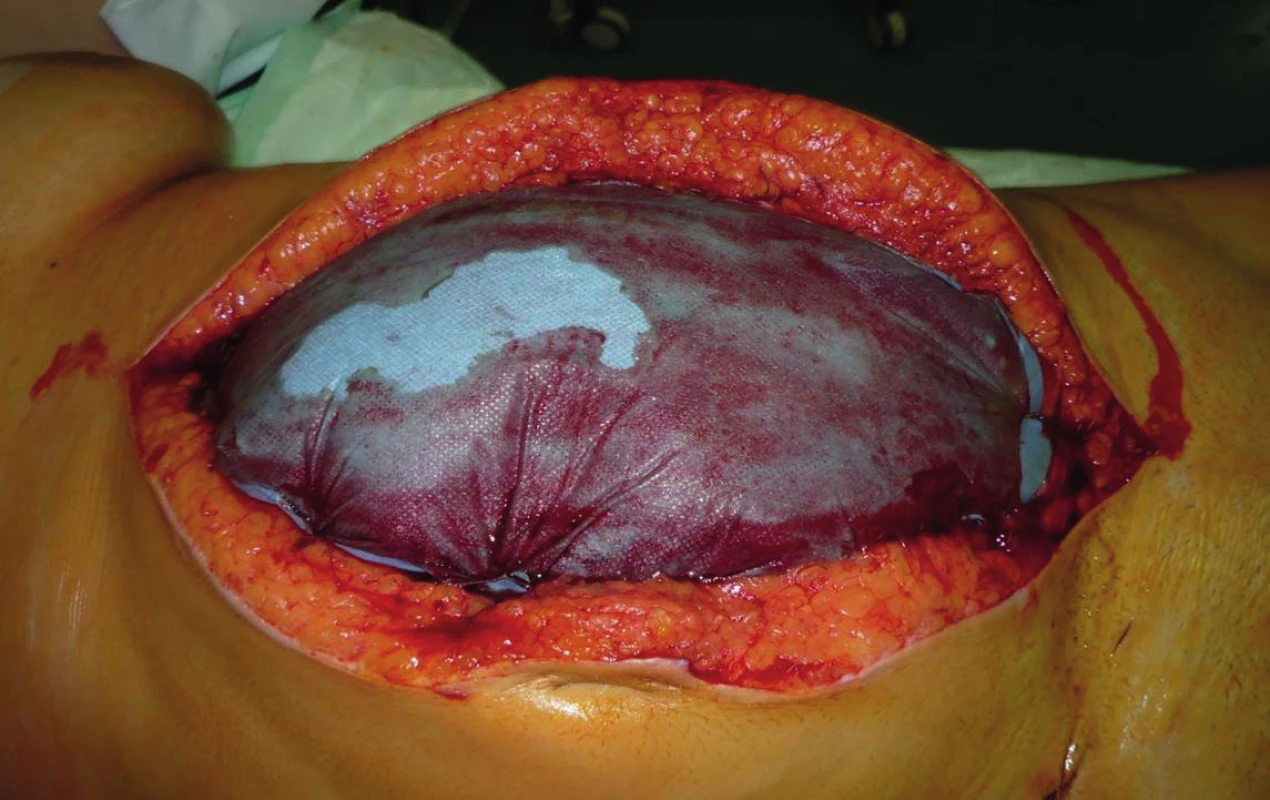
7. Laparostomy covered with “Steri-Drape” 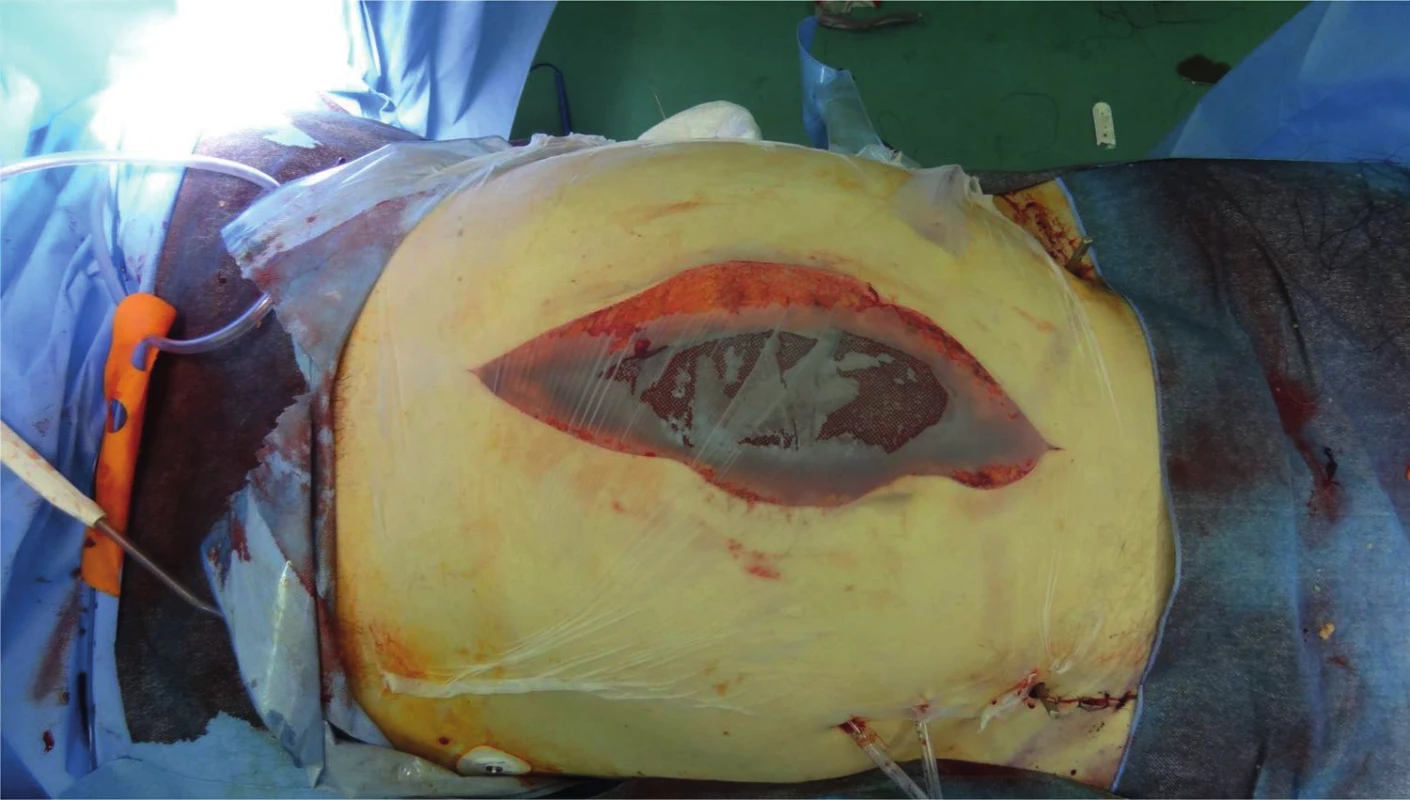
Decompressive laparostomy leads to a rapid restoration of oxygenation and pulmonary compliance, inspiration pressures are quickly normalized and diuresis is promptly restored [1]. Decompression of the abdominal cavity may be followed with a development of reperfusion syndrome, which may be manifested even with asystoly. The possible cause of this condition may be seen in a sudden decrease of peripheral vascular resistance, with subsequent serious hypovolemia [13], or release of anaerobic metabolites from hypoperfunded splachnic area. In order to minimize these symptoms, thorough correction of acidobasic balance and levels of electrolytes is recommended, and also volume pre-load of the circulation with two litres of saline and administration of Mannitol and bicarbonate prior to the procedure [5]. In patients, in whom a timely decompression was performed before a development of a significant organ failure, primary closure of the fascia may be performed in 5–7 days [8].
CONCLUSION
Developed abdominal compartment syndrome is a serious, life-threatening condition, requiring immediate surgical intervention. This complication must be considered not only in patients with a serious abdominal trauma but also in patients undergoing prolonged abdominal surgeries, with massive volume resuscitation [18]. In these patients, regular monitoring of the intraabdominal pressure is required. This is presently most easily performed by measuring the pressure in the urinary bladder. Elevation of IAP above 20 mmHg may be considered an indication for performance of decompressive laparostomy. However, it is not possible to base the reasoning about further course of treatment on the IAP values only; it is also necessary to observe clinical manifestations related to insufficient reaction to conservative therapy. Prominent distention of the abdominal wall is associated with ventilation insufficiency, elevation of ventilation pressures, circulatory instability and alteration of renal functions. These symptoms, even at the presence of borderline IAP values, should point us towards immediate surgical intervention – decompressive laparostomy. Surgical intervention may be inevitable, however only a last resort in providing care for patients threatened with ACS development. Already from the beginning of treatment, these patients require a complex multidisciplinary intensive care, which must include a maximum utilization of conservative procedures of IAP reduction. Placement of preventive primary laparostomy also belongs among procedures, which have a place in the treatment of patients with serious abdominal trauma.
Sources
1. Asensio, AJ., Trunkey, DD. Current Therapy of Trauma and Surgical Critical Care. Philadelphia: Mosby, 2008. 785 s. ISBN 978-0-323-04418-9.
2. Bloomfield, GL., Dalton, JM., Sugerman, HJ. et al. Treatment of increasing intracranial pressure secondary to the acute abdominal compartment syndrome in patient with combined abdominal and head trauma. J Trauma. 1995, 39, 1168 - 1170. ISSN 0022-5282.
3. Bongard, F., PIANIM, N., dubecz, s. et al. Adverse consequences of increased intraabdominal pressure on bowel tissue oxygen. J Trauma. 1995, 39, 519-524. ISSN 0022-5282.
4. De Waele, JJ., De Laet, I., De Keuleaner, B. et al. The effect of different reference transducer positions on intra-abdominal pressure maeasurement: a multicenter analysis. Intensive Care Med. 2008, 34, 1299-1303. ISSN 0342-4642.
5. Eddy, V., Nunn, C., Morris, JA. Abdominal compartment syndrome. The Nashville experience. Surg Clin North Am. 1997, 77, 801-812. ISSN 0039-6109.
6. Eleftheriadis, E., kotzaMPASSI, k., pAPANOTAS, k. et al. Gut ischaemia, oxidative stress, and bacterial translocation in elevated abdominal pressure in rats. World J Surg. 1996, 20,11-16. ISSN 0364-2313.
7. Hildebrand, F. , Pape, HC. Acute compartment syndrome. Eur J Trauma Emerg Surg. 2014, 40, 519-520. ISSN 1863-9933.
8. Cheatham, ML. Abdominal compartment syndrome. Curr Opin Crit Care. 2009, 15, 154-162. ISSN 1070-5295.
9. Cheatham, ML. Nonoperative management of intraabdominal hypertension and abdominal compartment syndrome. World J Surg. 2009, 33, 1116-1122. ISSN 0364-2313.
10. Cheatham, ML., Malbrain, ML., Kirkpatrick, A. et al. Results from the International conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. II. Recommendations. Intensive Care Med. 2007, 33, 951-962. ISSN 0342-4642.
11. Ivatury, RR., Porter, JM., Simon, RJ., et al. Intra-abdominal hypertension after life-threatening penetrating abdominal trauma: prophylaxis, incidence, and clinical relevance to gastric mucosal pH and abdominal compartment syndrome. J Trauma. 1998, 44, 1016-1021. ISSN 0022-5282.
12. Ivatury, RR., Diebel, l., porter, jm. et al. Intra-abdominal hypertension and the abdominal compartment syndrome. Surg Clin North Am. 1997, 77, 783-80. ISSN 0039-6109.
13. Kitka, M., Pleva, L. Poranenia orgánov brušnej dutiny. Košice : Klinika úrazovej chirurgie LF UJPŠ a FNLP, 2003. 71 s. ISBN 80-968824-5-7.
14. Kron, IL., harman, pk., nolan, sp. The measurement of intra-abdominal pressure as a criterion for abdominal re-exploration. Ann Surg. 1984, 199, 28-30. ISSN 0003-4932.
15. Malbrain, ML., Cheatham, ML., Kirkpatrick, A. et al. Results from the International conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. I. Definitions. Intensive Care Med. 2006, 32, 1722-1732. ISSN 0342-4642.
16. McBeth, PB., Zygun, DA., Widder, S. et al. Effect of patient positioning on intra-abdominal pressure monitoring. Am J Surg. 2007, 193, 644-647. ISSN 0002-9610.
17. Meldrum, DR., MOORE, FA., MOORE, EE. et al. Prospective characterization and selective management of the abdominal compartment syndrome. Am J Surg. 1997, 174, 667-673. ISSN 0002-9610.
18. Pleva, L., Mayzlík, J., Šír, M. Abdominální kompartment syndrom u polytraumatu. Úrazová chirurgie. 2003, 11, 7-12. ISSN 1211-7080
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2017 Issue 4-
All articles in this issue
- Surgical stabilization of chest wall –development of the method and contemporary trends
- Abdominal compartment syndrome in polytrauma
- Blunt liver and splenic trauma due to distal rib fracture
- Evaluation of medium-term outcomes of surgical treatment of talus neck fractures at the Department of Trauma Surgery, University Hospital Brno
- Trauma Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Abdominal compartment syndrome in polytrauma
- Blunt liver and splenic trauma due to distal rib fracture
- Surgical stabilization of chest wall –development of the method and contemporary trends
- Evaluation of medium-term outcomes of surgical treatment of talus neck fractures at the Department of Trauma Surgery, University Hospital Brno
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

