-
Medical journals
- Career
Acromioclavicular dislocation associated with scapular fractures – pathoanatomy of the injury
Authors: T. Strnad; J. Bartonicek; M. Tucek
Authors‘ workplace: Department of Orthopedics, 1st Faculty of Medicine, Charles University and the Central Military Hospital – University Military Hospital, Prague
Published in: Rozhl. Chir., 2022, roč. 101, č. 6, s. 273-277.
Category: Original articles
doi: https://doi.org/10.33699/PIS.2022.101.6.272–276Overview
Introduction: No detailed study dealing with an injury to the AC joint in combination with scapular fractures has been published to date. The aim of this study is to describe pathoanatomy of these injuries.
Methods: In a series of 519 scapular fractures in adult patients from the period of 2002−2020 we identified a total of 20 (3.9%) cases associated with AC dislocation. The group comprised 17 men and 3 women with the mean age of 49 years (range, 21−78). Radiographs of the shoulder joint followed by CT examination, including 3D reconstructions, were performed in all patients. This documentation allowed assessment of the scapular fracture pattern and type of injury to the AC joint.
Results: AC dislocation was associated with a simple scapular fracture in 15 cases (7 fractures of the coracoid base, 4 fractures of the acromion or the lateral spine, 2 fractures of the scapular body, 1 fracture of the superior and 1 fracture of the inferior glenoid). In 5 cases AC dislocation accompanied multiple or complex scapular fractures (once a combination of a coracoid fracture and a fracture of the lateral scapular spine, once a combination of a fracture of the superior glenoid and of the acromion, 2 cases of a complex intraarticular fracture and 1 case of scapulothoracic dissociation).
Conclusion: AC dislocation is relatively infrequent injury accompanying scapular fractures. It is most commonly associated with fractures of coracoid, acromion/lateral spine or superior glenoid. No case of AC dislocation was recorded in a fracture of the scapular neck.
Keywords:
fracture – scapular – acromioclavicular dislocation – pathoanatomy
INTRODUCTION
The incidence of acromioclavicular (AC) dislocation associated with scapular fractures is reported to be between 3% and 6% [1–3]. Probably the first case of AC dislocation combined with a scapular fracture, more specifically with separation of the coracoid, was discussed by Gurtl [4] in 1864. A more detailed study of this issue was published by Ehalt [5] in 1934. Since then, numerous cases of AC dislocation combined with scapular fractures, mainly those of the coracoid, but also with other scapular fracture patterns, have been described in the form of case reports [6-20]. However, no detailed study dealing with an injury to the AC joint in combination with scapular fractures has been published to date. The aim of this study is to describe pathoanatomy of these injuries.
METHODS
Material: In a series of 519 scapular fractures in adult patients from the period of 2002−2020 we identified a total of 20 (3.9%) cases associated with AC dislocation. The group comprised 17 men and 3 women with the mean age of 49 years (range, 21−78). The mean age of men was 48 years, that of women 61 years. The right side was involved in 8 cases, the left side in 12 cases. All the patients in the group were skeletally mature, with an acute injury to the AC joint and an acute scapular fracture.
Method: Radiographs of the shoulder joint followed by CT examination, including 3D reconstructions, were performed in all the patients. This documentation allowed assessment of the scapular fracture pattern and the type of injury to the AC joint.
Evaluation: The following parameters were examined:
- the scapular fracture pattern classified according to Bartoníček et al. [21],
- incidence rate of AC dislocation of the given type of the scapular injury,
- type of AC dislocation according to the Rockwood classification [22],
- the type of injury to the coracoclavicular junction.
RESULTS
Type of injury to the scapula: AC dislocation was recorded in fractures of the processes (coracoid, acromion), scapular body, glenoid, in complex fractures and scapulothoracic dissociation (STD).
AC dislocation was associated with a simple scapular fracture in 15 cases, i.e. 7 fractures of the coracoid base, 4 fractures of the acromion or the lateral spine, 2 fractures of the scapular body, 1 fracture of the superior and 1 fracture of the inferior glenoid (Fig. 1).
Fig. 1: A simple fracture of the scapula (coracoid fracture) associated with AC dislocation 
Radiograph a) and 3D CT reconstruction b). In 5 cases AC dislocation accompanied multiple or complex scapular fractures, i.e. once a combination of a coracoid fracture and a fracture of the lateral scapular spine, once a combination of a fracture of the superior glenoid and of the acromion, 2 cases of a complex intraarticular fracture (Fig. 2) and 1 case of STD.
Fig. 2: A complex intraarticular fracture of the scapula associated with AC dislocation 
Radiograph a) and 3D CT reconstruction b). AC dislocation was most frequently combined with fractures of the processes (14 cases), no case of AC dislocation was recorded in fractures of the scapular neck (Tab. 1).
1. Basic characteristics of the cohort of patients with AC dislocation 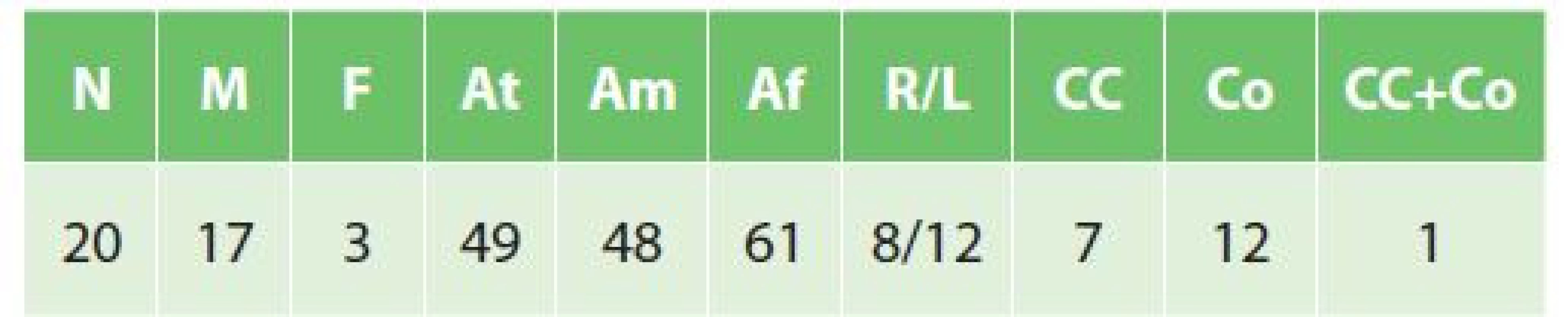
Legend: M – males; F – females, At – mean age of the whole cohort; Am – mean age of men; Af – mean age of women; R– right side; L – left side; CC – rupture of the coracoclavicular ligament; Co – fracture of the coracoid; CC+Co – rupture of the coracoclavicular ligament associated with a fracture of the coracoid. Relative incidence of AC dislocation in individual types and subtypes of scapular fractures is shown in Tab. 2 and 3.
2. Incidence of AC dislocation in individual scapular fracture patterns 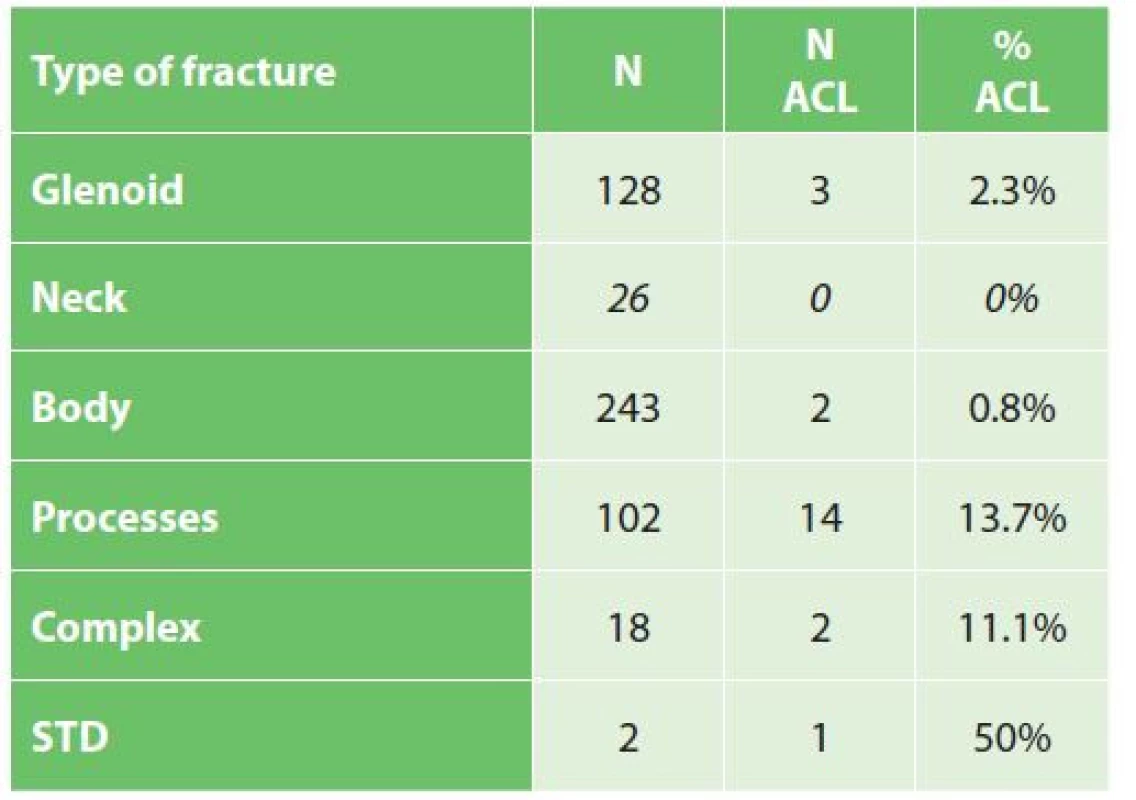
Legend: N – number of cases, ACL – acromioclavicular dislocation. 3. Tab. 3: Incidence of AC dislocation in individual fracture subtypes 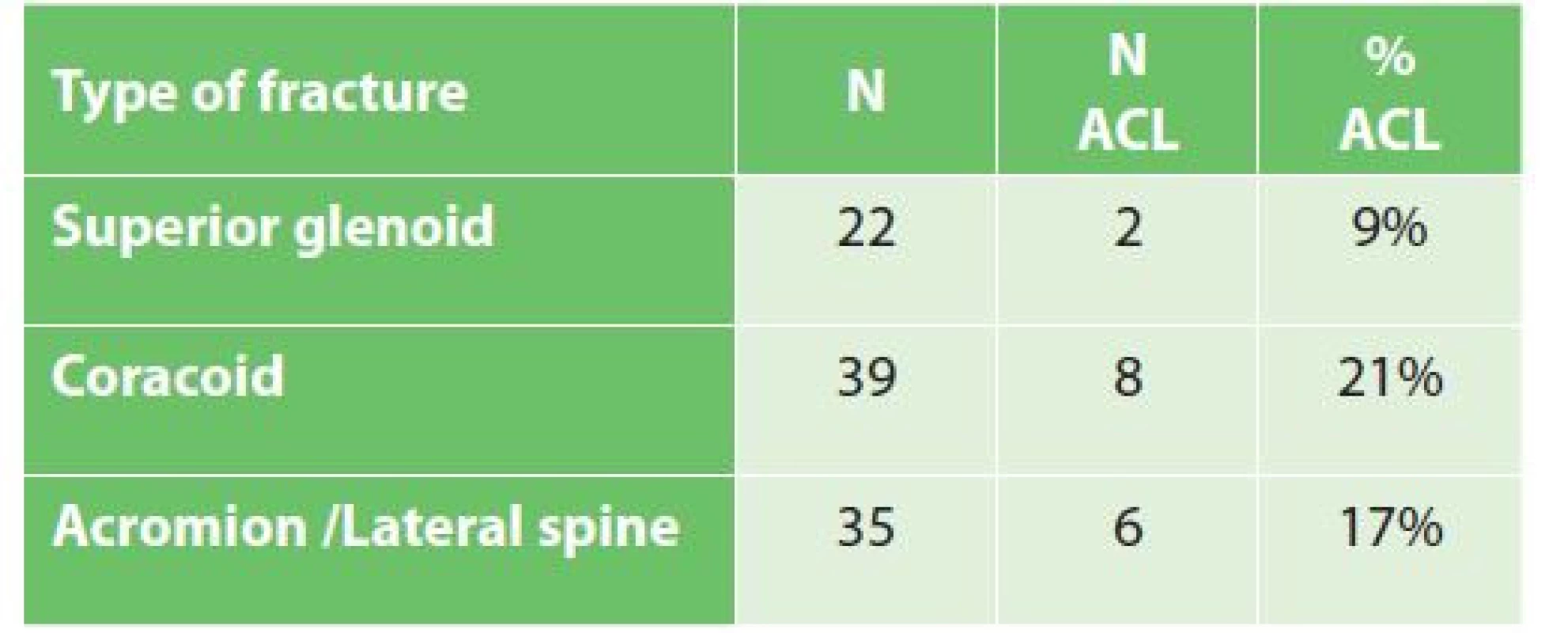
Legend: N – number of cases, ACL – acromioclavicular dislocation. Types of AC dislocation: Rockwood type III was recorded in 12 cases, type IV in 5 cases, including 1 case combined also with dislocation of the SC joint, type V in 2 cases (Fig. 3); and in 1 case of STD there occurred only distraction of the AC joint (Fig. 4).
Fig. 3: Various types of AC dislocation on 3D CT reconstructions 
a) type III associated with a coracoid fracture; b) type IV associated with an acromion fracture; c) type V associated with a fracture of the superior glenoid. Fig. 4: Distraction of the AC joint associated with SC dislocation in scapulothoracic dissociation on 3D CT reconstructions 
Type III was associated with a fracture of the coracoid base in 5 cases, with a scapular body fracture in 2 cases, a complex intraarticular fracture in 2 cases, a comminuted fracture of the coracoid and the lateral spine in 1 case, a fracture of the inferior glenoid in 1 case and a fracture of the superior glenoid and acromion in 1 case. Type IV was recorded in 4 cases in combination with a fracture of the acromion or the lateral spine and in 1 case in association with a fracture of the coracoid base. Type V was identified in 1 case in a fracture of the coracoid base and in 1 case in a fracture of the superior glenoid with a concomitant rupture of the coracoclavicular ligament.
Type of injury to the coracoclavicular junction: Rupture of the coracoclavicular ligament was identified in 7 cases, causing ligamentous instability, combined with a fracture of the acromion or the lateral spine in 4 cases, a fracture of the scapular body in 2 cases (Fig. 5) and a fracture of the inferior glenoid in 1 case (Fig. 6).
Fig. 5: Ligamentous instability of the coracoclavicular junction in a fracture of the infraspinous part of the scapular body on radiograph 
Fig. 6: Ligamentous instability of the coracoclavicular junction in a fracture of the inferior glenoid on radiograph 
In 11 cases the coracoclavicular ligament remained intact; however, separation of the coracoid or the superior glenoid resulted in osseous instability (Fig. 1): 7 cases were an isolated extraarticular fracture of the coracoid base, 1 case a comminuted fracture of the coracoid associated with a fracture of the lateral spine, 1 case a combination of a fracture of the superior glenoid and the acromion. In 2 complex intraarticular fractures AC instability was caused by separation of the superior glenoid.
In 2 cases there occurred combined osseous-ligamentous instability, including 1 case of rupture of the coracoclavicular ligament and fracture of the superior glenoid (Fig. 7) and 1 case rupture of the coracoclavicular ligament and fracture of the coracoid base as part of STD.
Fig. 7: A combined osseous-ligamentous instability of the coracoclavicular junction in a fracture of the superior glenoid associated with rupture of the coracoclavicular ligament 
Overall, rupture of the coracoclavicular ligament occurred in 9 cases, separation of the coracoid in 9 cases and fracture of the superior glenoid in 4 cases.
DISCUSSION
To date, injuries to the AC joint have been mentioned only marginally in larger studies of scapular fractures [1−3,16,17,19]; more details can be found only in individual case reports [6−15,18,20]. Thus our study is the first to deal with this issue in detail. Analysis has shown that AC dislocation is a relatively infrequent complication of scapular fractures, with the incidence of less than 4%. AC dislocation accompanies most often fractures of the processes of the scapula (coracoid, acromion or the lateral scapular spine) or fractures of the superior glenoid, either isolated or occurring as part of complex intraarticular fractures of the scapula.
Fractures of the coracoid and the superior glenoid disrupt integrity of the coracoclavicular junction and are a direct cause of AC dislocation. This finding is in case of a fracture of the coracoid base important also from the viewpoint of treatment, because reduction and internal fixation of the coracoid stabilizes also AC dislocation. And, vice versa, reduction and stabilization of AC dislocation may lead to indirect reduction and healing of the coracoid fracture. Fractures of the superior glenoid should be assessed in terms of displacement and on this basis preferable treatment, i.e., open reduction and internal fixation or a mere reduction and stabilization of the AC joint, should be used.
An interesting finding in our cohort was combined osseous-ligamentous instability resulting from disruption of the coracoclavicular junction at two levels. Such a lesion has not been reported in the literature, yet.
CONCLUSION
AC dislocation is a relatively infrequent injury accompanying scapular fractures. It is most commonly associated with fractures of the coracoid, acromion/ lateral spine or superior glenoid. No case of AC dislocation was recorded in fractures of the scapular neck. The coracoclavicular junction is more often affected by osseous instability caused by fracture of the coracoid base or the superior glenoid than by ligamentous instability resulting from rupture of the coracoclavicular ligament. Combined osseous-ligamentous instability is rare.
Conflict of interests
The authors declare that they have not conflict of interest in connection with this paper and that the article has not been published in any other journal, except congress abstracts and clinical guidelines.
MUDr. Tomáš Strnad
Klinika ortopedie 1. LF UK UVN – FVN Praha
e-mail: tomas.strnad@uvn.cz
ORCID: 0000-0001-5021-1031
Sources
1. McGahan JP, Rab GT, Dublin A. Fractures of the scapula. J Trauma 1980;20(10):880−883. doi: 10.1097/00005373-198010000-00011.
2. Armstrong CP, Van der Spuy J. The fractured scapula: importance and management based on a series of 62 patients. Injury 1984;15(5):324−329. doi: 10.1016/0020-1383(84)90056-1.
3. Ada JR, Miller ME. Scapula fractures. Analysis of 113 cases. Clin Orthop Relat Res. 1991;269 : 174−180.
4. Gurtl E. Handbuch der Lehre von den Knochenbrüchen. Zweiter Teil. Hamm, Grote 1864 : 521−540.
5. Ehalt W. Luxatio acromioclavicularis mit gleichzeitigem Abriss des Processus coracoideus scapulae. Arch Orthop Trauma Surg. 1934;34 : 421−425. doi: 10.1007/ BF02580532.
6. Urist MR. Complete dislocation of the acromioclavicular joint; the nature of the traumatic lesion and effective methods of treatment with an analysis of forty-one cases. J Bone Joint Surg Am. 1946;28(4):813−837.
7. Allman FL. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am 1967;49(4):774−784.
8. Lasda NA, Murray DG. Fracture separation of the coracoid process associated with acromioclavicular dislocation. Clin Orthop Relat Res. 1978;134 : 222−224.
9. Bernard TN Jr., Brunet ME, Haddad RJ Jr. Fractured coracoid process in acromioclavicular luxation. Report of four cases and review of the literature. Clin Orthop Relat Res. 1983;175 : 227−232.
10. Carr AJ, Broughton NS. Acromioclavicular dislocation associated with fracture of the coracoid process. J Trauma 1989;29(1):125−6. doi: 10.1097/00005373-198901000-00030.
11. Wilson KM, Colwill JC. Combined acromioclavicular dislocation with coracoclavicular ligament disruption and coracoid process fracture. Am J Sports Med. 1989;17(5):697−698. doi: 10.1177/036354658901700521.
12. Wang KC, Hsu KY, Shih CH. Coracoid process fracture combined with acromioclavicular dislocation and coracoclavicular ligament rupture. Clin Orthop Relat Res. 1994;300 : 112−122.
13. Kurdy NMG, Shah SV. Fracture of the acromion associated with acromioclavicular dislocation. Injury 1995;26(9):636−637. doi: 10.1016/0020-1383(95)00117-r.
14. DiPaola M, Marchetto P. Coracoid process fracture with acromioclavicular joint separation in an American football player: A case report and literature review. Am J Orthop. 2009;38(1):37−40.
15. Duan X, Zhang H, Zhang H, et al. Treatment of coracoid process fractures associated with acromioclavicular dislocation using clavicular hook plate. J Shoulder Elbow Surg 2010;19(2):e22−5. doi: 10.1016/j.jse.2009.09.004.
16. Bartoníček J, Frič V. Scapular body fractures: Results of the operative treatment. Int Orthop. 2011;35(5):747−53. doi: 10.1007/s00264-010-1072-y.
17. Cole PA, Gauger EM, Herrera DA, et al. Radiographic follow-up of 84 operatively treated scapula neck and body fractures. Injury 2012;43(3):327−333. doi: 10.1016/j. injury.2011.09.029.
18. Allagui M, Koubaa M, Aloui I, et al.Coracoid fracture combined with distal clavicle fracture without coracoclavicular ligament rupture: A case report. J Clin Orthop Trauma 2013;4(4):190−193. doi: 10.1016/j.jcot.2013.10.002.
19. Asci M, Gunes T, Bilgie E, et al. Concurrent AC joint dislocation, coracoclavicular ligament rupture and coracoid base fracture. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2206−2208. doi: 10.1007/s00167-015-3524-9.
20. Tatro JM. Gilbertson JA, Schroder LK, et al.Five to ten-year outcomes of operatively treated scapular fractures. J Bone Joint Surg Am 2018;100(10):871−878. doi: 10.2106/JBJS.17.00673.
21. Bartoníček J. Scapular fractures. In: Tornetta P, Ricci WM, Ostrum RF, et al. Rockwood and Green´s Fractures in Adults. 9th ed. Philadelphia, Wolters Kluwer 2020 : 976−1008.
22. Rockwood CA. Injuries to the acromioclavicular joint. In: Rockwood, Green DP. Fractures in adults. Vol 1. 2nd ed. Philadelphia, JB Lippincott 1984 : 860−910.
Labels
Surgery Orthopaedics Trauma surgery
Article was published inPerspectives in Surgery
2022 Issue 6-
All articles in this issue
- Je defenzivní medicína problémem chirurgů?
- Defensive medicine and the influence of litigation on doctors
- Retroperitoneal fibrosis – diagnosis and treatment
- Bilateral versus unilateral total knee replacement – comparison of clinical and functional results in two-year follow-up
- Delayed diagnosis of diaphragmatic rupture after blunt chest trauma – 2 case reports
- Omental torsion as a rare cause of pain in the right subcostal space – a case report
- Atraumatic acute compartment syndrome – case report
- Acromioclavicular dislocation associated with scapular fractures – pathoanatomy of the injury
- Perspectives in Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Retroperitoneal fibrosis – diagnosis and treatment
- Atraumatic acute compartment syndrome – case report
- Defensive medicine and the influence of litigation on doctors
- Bilateral versus unilateral total knee replacement – comparison of clinical and functional results in two-year follow-up
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

