-
Medical journals
- Career
The optic nerve drusen and haemodynamics
Authors: J. Čmelo 1; J. Valašková 2; V. Krásnik 2
Authors‘ workplace: Centrum neurooftalmológie, Bratislava, doc. MUDr. Jozef Čmelo, Ph. D., MPH. 1; Klinika Oftalmológie LF UK a UNB, Prednosta: doc. MUDr. Vladimír Krásnik, Ph. D. 2
Published in: Čes. a slov. Oftal., 75, 2019, No. 5, p. 252-256
Category: Original Article
doi: https://doi.org/10.31348/2019/5/2Overview
Purpose: The optic nerve drusen (DON) are precisely described in many papers. But fewer papers evaluate real haemodynamics parameters (HP) in DON. Clinically, it has been shown, that the development and progression of visual field changes in DON is closely related to the hemodynamics of the ocular vascular supply - the optic nerve. DON can visually overlap the excavation optic disc, making it difficult to evaluate scotomas of the visual field in glaucoma.
Methods: HP was prospectively evaluated in 54 patients with compensated intraocular pressure and DON. The drusen at the optic nerve head have been detected by fundus examination and B-scan ultrasonography (USG). DON were divided into 3 groups according to the size of the individual drusen or the drusen complex. I. Group: area size up to 1.9 mm. II. Group: area size: 1.9 - 3.9 mm. III. Group: area size: ≥ 4,0 mm. HP - maximum systolic velocity (MSV), minimal diastolic velocity (MDV) and resistance indices (IR) and index pulsatility (IP) - were recorded at the central retinal artery (CRA), at the central retinal vein (CRV), at ciliares posteriores arteries breves (CPAb) and at the ophthalmic artery (AO). The values were divided into 3 groups: 1 - Physiological: CRA: 8.7 ± 0.9 / 2.9 ± 0.6 cm/s or RI: 0.70 ± 0.05. 2 - Slightly impaired: CRA: 6.6 ± 0.8 / 2.0 ± 0.5 cm/s, or RI: 0.75 ± -0.04. 3 - Significantly impaired: CRA: 5.2 ± 1.2 / 1.9 ± 0.7 cm/sec or RI: 0.79 ± 0.03.
Results: There was no linear relationship between size of DON and HP. Slight worsening of HP at the CRA was in I. Group (28.6 %), II. Group (48.3 %) and III. Group (62.4 %). Significant worsening of HP at the CRA was I. group (28.6 %), II. Group (48.3 %) and in III. Group (62.4 %). HP of the CPA and of the OA were not significant due to the presence and size of drusen. The relationship between individual variables was evaluated using the Pearson correlation coefficient 0.213. I. Group P: 0.354, II. Group P: 0.073, III. Group P: 0.287.
Conclusions: HP is more often impaired in „large“ DON (Group III), rarely in Group I, but this is not a rule. HP cannot be predicted according to the size of the druse formation at the optic nerve. It seems that the deterioration of HP depends not only on the DON size but also on the location (the distance from the lamella cribriformis) and also to the vascular system intrapapillary.
Keywords:
glaucoma – haemodynamics – drusen optic nerve – visual field – flow parameters – Doppler ultrasonography
INTRODUCTION
With the development of imaging techniques, the diagnostics (dg) of many pathologies of the optic nerve is also improving. These include optic disc drusen (ODD).
It has been clinically demonstrated that the occurrence and progression of changes in the visual field in the case of ODD is closely related to the haemodynamics of vascular supply to the eye – the optic nerve (7, 9). The problem of ODD has been described in detail in several publications and observations. However, less attention has been devoted to real haemodynamic changes in the optic nerve in ODD. In ODD it has been both experimentally and clinically demonstrated that the haemodynamic parameters are impaired. However, a more serious issue is that progression of changes in the visual field has likewise been demonstrated. ODD may visually overlap excavation of the disc of the optic nerve, on the basis of which it is more difficult to evaluate changes (scotomas) in the visual field in the case of glaucoma.
METHOD
A prospective evaluation was conducted on 54 patients with bilateral or unilateral optic disc drusens. The patients had stabilised blood pressure and pulse, intraocular pressure was 11-19 torr. Diabetics and patients with glaucoma and untreated or uncompensated hypertension were excluded. The presence of drusens in the head of the optic nerve was demonstrated by means of a fundus examination (Fig. 1) and B-scan ultrasonography (USG). For more precise measurement and to minimise the “halo” effect in USG imaging, the value of acoustic imaging (“Gain”) was minimised to 5 dB (Fig. 2).
1. Photograph of a large complex of optic disc drusens 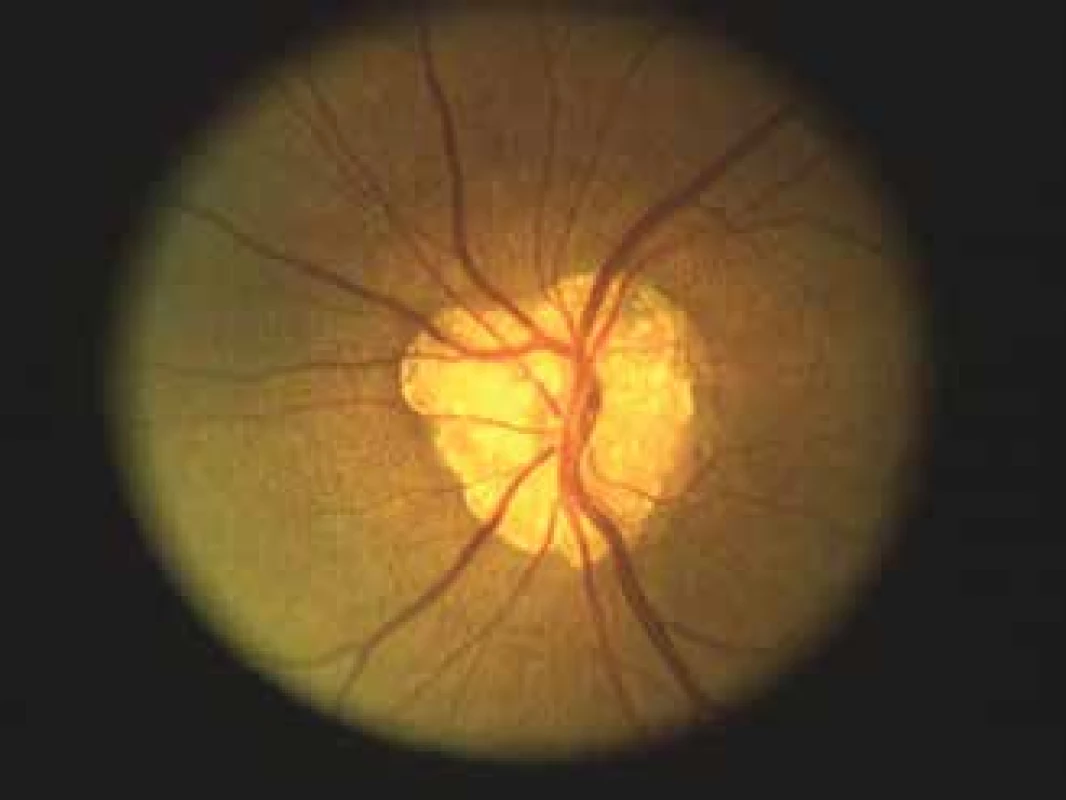
2. Left: Optic disc drusens B-scan ultrasonography in standard mode – gain 59 dB. Right: “halo” effect of optic disc drusens is minimised (drusens display in actual size) when gain is reduced to 0 dB. 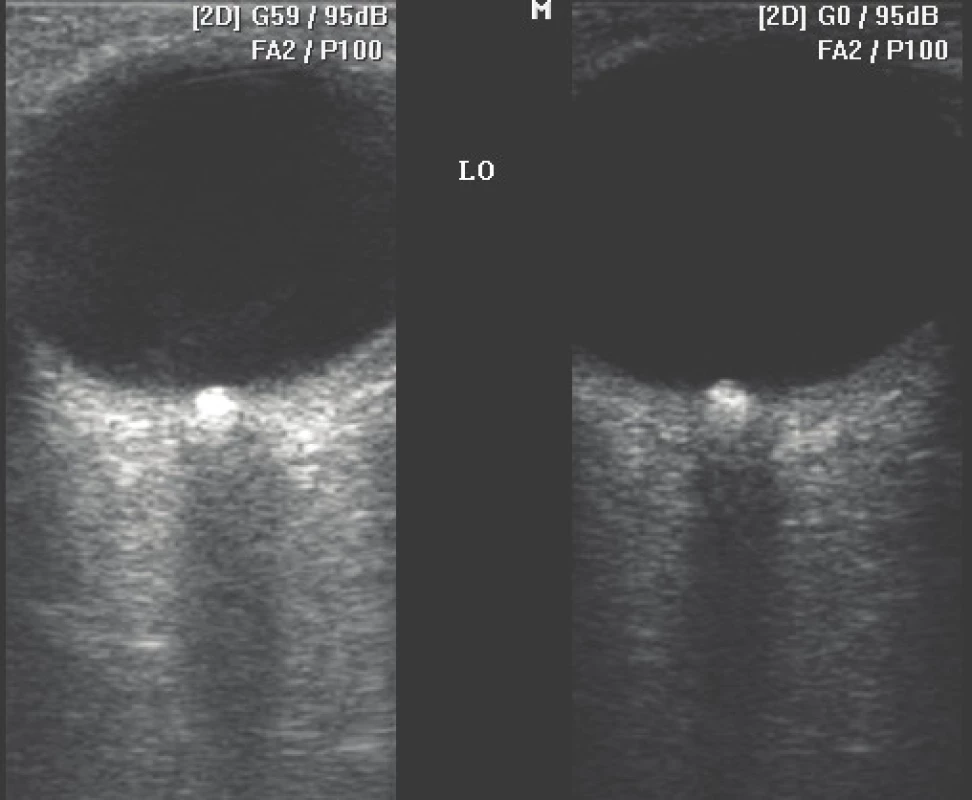
Drusens were divided into 3 groups according to summary size. Area size of the drusens according to USG imaging was taken into consideration. In the case of occurrence of multiple drusens within the framework of a single optic nerve (drusen complex), the total surface area was determined by the sum of the individual drusens. Group I: ophthalmoscopically invisible + visualisation only with the aid of ultrasonography, area size up to 1.9 mm. Group II: area size: 1.9-3.9 mm (Fig. 3). Group III: area size > 4.0 mm.
3. USG imaging B-scan of optic disc drusens – Group III (according to size) 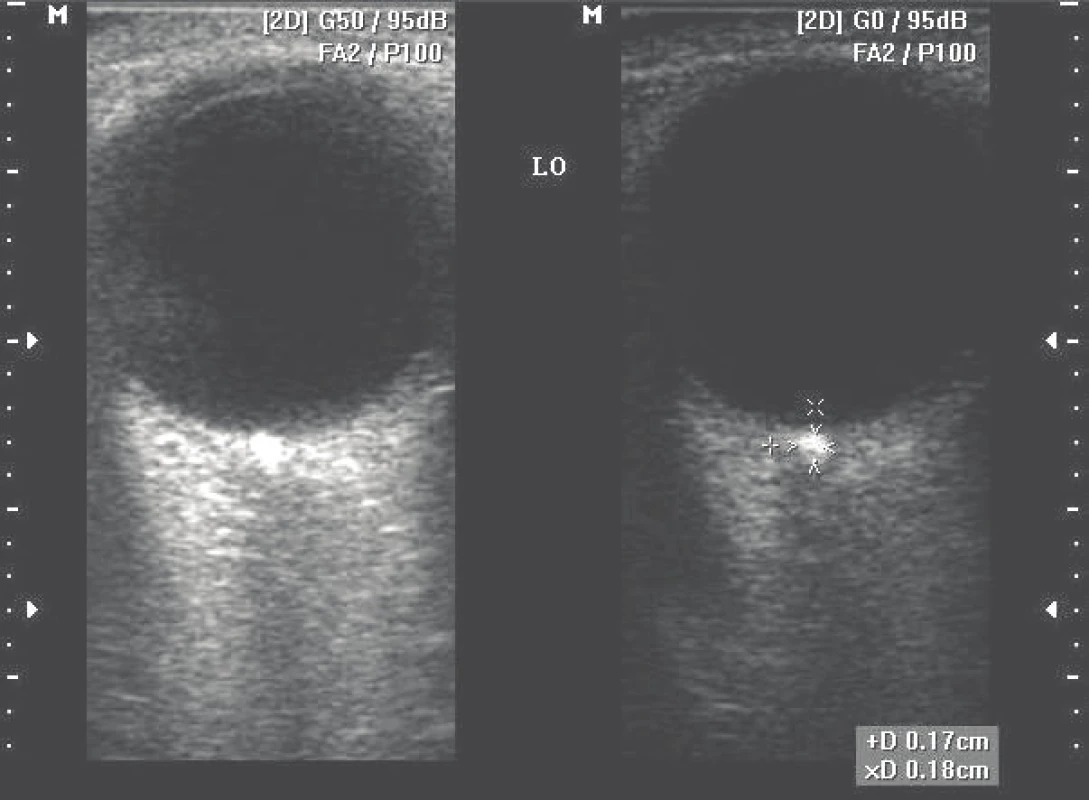
Haemodynamic parameters (HP) were recorded in the central retinal artery (CRA) (Fig. 4), in the central retinal vein (CRV), in the temporal and nasal ciliares posteriores arteries breves (CPAb) and in the ophthalmic artery (OA). The evaluated parameters were maximum systolic velocity (MSV), minimum diastolic velocity (MDV) and resistivity index (RI) and pulsatility index (PI), indicating the state of peripheral resistance from the place of detection.
4. Colour Doppler ultrasonography – pronouncedly low flow parameters in central retinal artery 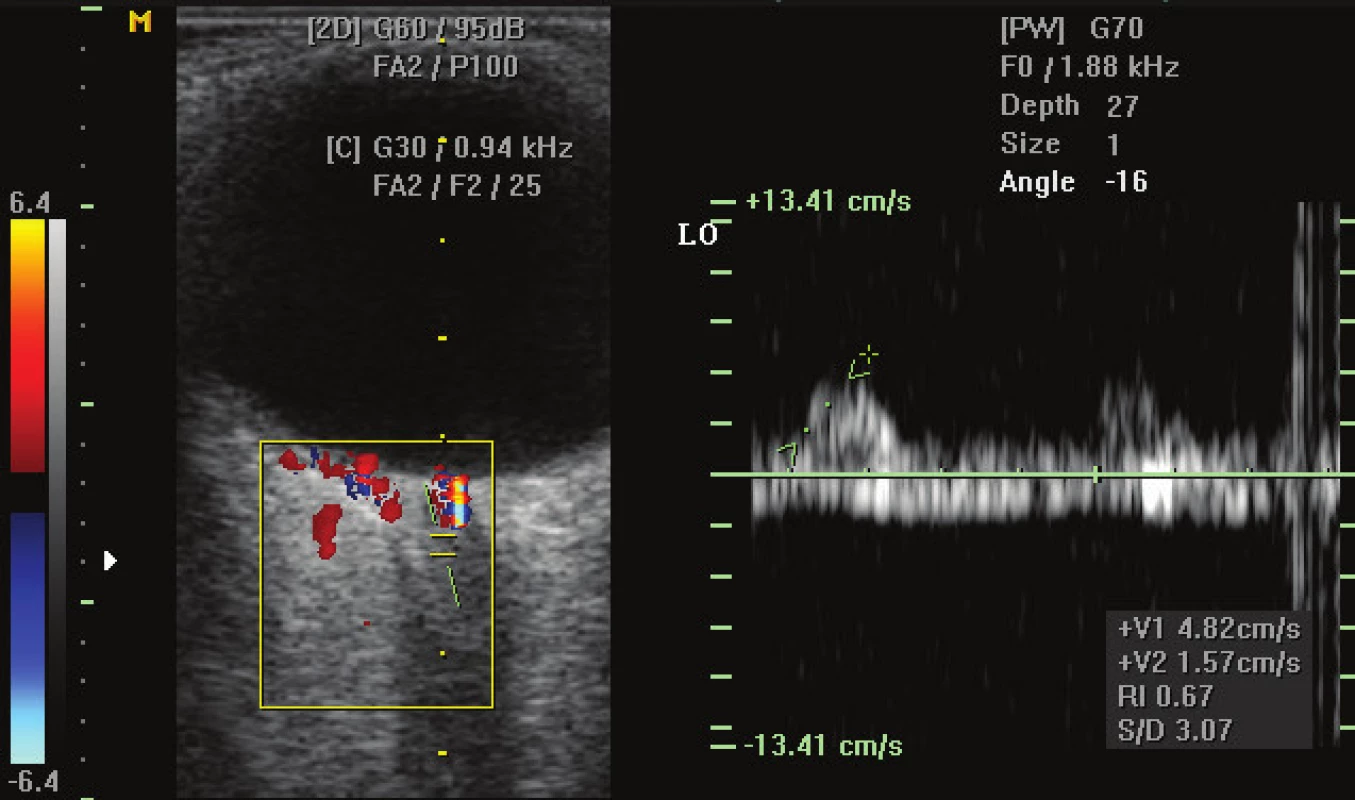
The values were divided into 1. Physiological: CRA: 8.7 ± 0.9 / 2.9 ± 0.6 cm/s, or RI: 0.70 ± 0.05, 2. Slightly impaired: CRA: 6.6 ± 0.8 / 2.0 ± 0.5 cm/s, or RI: 0.75 ± 0.04. 3. Significantly impaired: CRA: 5.2 ± 1.2 / 1.9 ± 0.7 cm/s, or RI: 0.79 ± 0.03. The relationship between the individual variables was evaluated with the aid of a Pearson correlation coefficient.
RESULTS
No linear relationship was demonstrated between the size of the drusens and flow (haemodynamic) parameters. Slightly impaired or significantly impaired HP in ODD was typified by an equal reduction of flow parameters in the CRA and CRV for example in comparison with glaucoma and other clinical findings. Significant impairment of HP in the CRA was present in 28.6% of group I drusens, 48.3% in group II and 62.4% in group III.
HP in the CPAb and OA were not of significant importance with regard to the presence and size of the drusens. The relationship between the individual variables was evaluated with the aid of a Pearson correlation coefficient: 0.213, group I P: 0.354, group II P: 0.073, group III P: 0.287.
DISCUSSION
From a histological perspective ODDs are calcified hyaline deposits accumulated on the inner side of the lamina cribriformis (from the vitreous body), and occur in approximately 3.5-5% of people (6, 13), 0.3-0.5% (2, 9, 15, 16). They appear at a young age, and change in size only rarely in adulthood. They are mostly diagnosed by chance. Subjectively ODDs are mostly asymptomatic. Sometimes various subjective changes of the visual field are manifested (constriction of visual field, transitory scotomas).
It is very important to differentiate ODD from other pseudo-edema, edema of the disc of the optic nerve, as well as oncological pathology, either primary or following preceding irradiation of an ocular tumour (6). Diagnosis is based on imaging of ODD with the aid of ophthalmoscopy, OCT examination, autofluorescence, computer tomography and USG. The most conclusive dg so far is ultrasonography in B-mode (1, 4, 5, 10, 13, 21).
Diagnosis of ODD is significant not only from the perspective of description (differential diagnosis of papilloedema), but also for timely identification of potential accompanying complications: disorders of the visual field, haemorrhages, increased risk of occlusive pathologies – non-arterial anterior ischemic neuropathy, branch central retinal vein occlusion, central retinal artery occlusion, choroidal neovascular membrane, changes in the retinal capillaries or differentiation of concurrent glaucoma damage (8, 15, 18, 23). Didactically it is possible to divide ODD according to various criteria. For example, according to Gripp (6) in terms of the number of displayed drusens in the head of the optic nerve, according to topography with regard to the lamina cribriformis. We selected division according to area size, which can be verified on various USG instruments.
It is very important and at the same time difficult to differentiate changes in the visual field in ODD and in the case of glaucoma (20). If diagnosis of ODD with the aid of B-scan ultrasonography is sufficiently processed, the real flow parameter in ODD requires relatively little work (3, 9, 12, 19). In the past the prevailing opinion was that examination with the aid of colour Doppler ultrasonography was not possible in the case of ODD (22). The study conducted by Pinto et al., as well as our experience, indicates that in the majority of cases this is possible without problems upon an appropriate inclination of the USG probe and setting of reading parameters in Color Doppler.
It is suitable to take the flow parameters as a part of the haemodynamics of the optic nerve, because they represent only a part of the complicated complex of blood supply of the optic nerve. Impairment of the flow parameters is illustrated not only by an increase in peripheral resistance (increase of resistivity index), but also by slowing of the current flow speed to beneath the physiological norm.
An interesting finding was that although significant and thus also risk impairment of HP was mostly in the largest drusen complexes, this was not an absolute rule. For this reason it would be suitable to evaluate also HP of the optic nerve in patients with ODD and progressive changes of the visual field.
CONCLUSION
Haemodynamic parameters are generally more often impaired in the case of “large” optic disc drusens (group III), and less frequently in group I ODDs – though this is not an absolute rule.
It appears that impairment of the haemodynamic parameters is conditioned not only by the size of the ODD, but also by the locality (distance from lamina cribriformis) and also the intrapapillary relationship to the vascular system. It is not possible to predict haemodynamic parameters according to the size of the drusen formation in the optic nerve. Evaluation of the real flow parameters should be a component of the examination of each patient with ODD who has progressive changes in the visual field.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received: 22. 7. 2019
Accepted: 26. 10. 2019
Available on-line: 17. 2. 2020
doc. MUDr. Jozef Čmelo, Ph.D., MPH.
Centrum neurooftalmológie,
Palas-Eye s.r.o.
Škultétyho 1
831 03 Bratislava,
Slovensko
Sources
1. Almog, Y., Nemet, A., Nemet, AY.: Optic disc drusen demonstrate a hyperechogenic artifact in B mode ultrasound. J Clin Neurosci, 23; 2016 : 111–119.
2. Auw-Haedrich, C., Staubach, F., Witschel, H.: Optic disk drusen. Surv Ophthalmol, 47; 2002 : 515–532.
3. Berenberg, TL., Metelitsina, TI., Madow, B. et al.: The Association Between Drusen Extent and Foveolar Choroidal Blood Flow in Age-Related Macular Degeneration. Retina, 32; 2012 : 25–31.
4. Boldt, HC., Byrne, SF., DiBernardo, C.: Echographic evaluation of optic disc drusen. J Clin Neuroophthalmol, 11; 1991 : 85–91.
5. De La Hoz Polo, M., Torramilans Luis, A., Pozuelo Segura, O. et al.: Ocular ultrasonography focused on the posterior eye segment: what radiologists should know. Insights Imaging, 7; 2016 : 351–364.
6. Furdová, A., Furdová, A., Krčméry, V.: Our experience with smartphone and spherical lens for the eye fundus examination during humanitarian project in Africa. Int J Ophthalmol, 10; 2017 : 157–160.
7. Grippo, TM., Shihadeh, WA., Schargus, M., Gramer, E. et al.: Optic Nerve Head Drusen and Visual Field Loss in Normotensive and Hypertensive Eyes. J Glaucoma, 17; 2008 : 100-104.
8. Hauptvogelová, M., Šustykevičová, Z.: Non-arteritická predná ischemická optická neuropatia pri drúzach zrakového nervu. Cesk Slov Oftalmol, 66; 2010 : 184–187.
9. Hendrix, W., Stalmans, I., Van Calster, J. et al.: Acute visual field constriction in optic disc drusen: report of an unusual case. Bull Soc Belge Ophtalmol; 2007 : 31-36.
10. Hlinomazová, Z., Hrazdíra, I.: Standardisation in ultrasonography: Principle and diagnostic significance. In ACTA MEDICA, 2/47. Hradec Králové, LF a UK Hradec Králové, 2004. S. 305-308.
11. Chang, MY., Pineles, SL.: Optic disk drusen in children. Surv Ophthalmol, 61; 2016 : 745–758.
12. Jianu, SN.: Color Doppler ecography in the study of retrobulbar circulation changes caused by optic nerve drusen. Oftalmologia, 53; 2009 : 74-80.
13. Kurz-Levin, MM., Landau, K.: A comparison of imaging techniques for diagnosing drusen of the optic nerve head. Arch Ophthalmol, 117; 1999 : 1045–1049.
14. Lee, KM., Woo, SJ., Hwang, JM.: Factors associated with visual field defects of optic disc drusen. PLoS ONE [online]. 2018. Dostupné na: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0196001
15. Lešták, J., Nutterová, E., Pitrová, Š. et al.: High Tension Versus Normal Tension Glaucoma. A comparison of Structural and Functional Examinations. J Clinic Experiment Opthalmol [online]. 2012. Dostupné na https://www.omicsonline.org/a-comparison-of-structural-and-functional-examinations-2155-9570.S5-006.php?aid=5007
16. Malmqvist, L., Li, XQ., Eckmann, C.L. et al.: Optic disc drusen in children: the Copenhagen Child Cohort 2000 Eye Study. J Neuroophthalmol, 38; 2017 : 140-146.
17. Noval, S., Visa J, Contreras I.: Visual field defects due to optic disk drusen in children. Graefes Arch Clin Exp Ophthalmol, 521/10; 2013 : 2445–2450.
18. Pilat, AV., Proudlock, FA., McLean, RJ. et al.: Morphology of retinal vessels in patients with optic nerve head drusen and optic disc edema. Invest Ophthalmol Vis Sci, 55/6; 2014 : 3484–3490.
19. Pinto, LA., Vandewalle, E., Marques-Neves, C. et al.: Visual field loss in optic disc drusen patients correlates with central retinal artery blood velocity patterns. Acta Ophthalmol, 92/4; 2014 : 286-291.
20. Skorkovská, K.: Perimetrie. Praha, Grada Publishing a.s., 2015, 116 s.
21. Štrofová, H., Jarošová, A.: Drúzy papily zrakového nervu a jejich komplikace. Cesk Slov Oftalmol, 72; 2016 : 298–308.
22. Ustymowicz, A., Obuchowska, I., Krejza, J. et al.: Limitations of color Doppler sonography in the imaging of ocular vessels. Eur J Ophthalmol, 14; 2004 : 584-587.
23. Žiak, P., Jarabáková, K., Koyšová, M.: Drúzová papila – súčasné diagnostické možnosti. Cesk Slov Oftalmol, 70; 2014 : 30-35.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 5-
All articles in this issue
- Vodiace psy sa cvičia na Slovensku už 25 rokov
- The long-term monitoring of sympathetic ophthalmia in the diagnostic and terapeutic view. Review Department of Ophthalmology
- The optic nerve drusen and haemodynamics
- Sensitivity and specificity of spectral OCT in patients with early glaucoma.
- Nanolaser in cataract surgery and its impact on corneal endotelium
- Molecular genetic cause of achromatopsia in two patients of Czech origin
- INTRAVITREAL THERAPY OF ENDOGENOUS ENDOPHTALMITIS DUE TO UROSEPSIS – A CASE REPORT
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Molecular genetic cause of achromatopsia in two patients of Czech origin
- INTRAVITREAL THERAPY OF ENDOGENOUS ENDOPHTALMITIS DUE TO UROSEPSIS – A CASE REPORT
- Sensitivity and specificity of spectral OCT in patients with early glaucoma.
- The long-term monitoring of sympathetic ophthalmia in the diagnostic and terapeutic view. Review Department of Ophthalmology
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


