-
Medical journals
- Career
Torpédo makulopatia. Kazuistika
Authors: Z. Šulavíková 1; V. Krásnik 2
Authors‘ workplace: Očná klinika, Fakultná nemocnica Trenčín 1; Klinika oftalmológie LFUK a UNB, Bratislava 2
Published in: Čes. a slov. Oftal., 79, 2023, No. 5, p. 268-238
Category: Case Report
doi: https://doi.org/10.31348/2023/31Overview
Aim: Torpedo maculopathy is an incidental, congenital retinal lesion. The typical clinical finding is a unilateral, symmetric, oval, hypopigmented lesion in the inferotemporal macula. In most cases, the lesion is along the horizontal raphe, is torpedo-shaped, and the nasal edge is directed into the foveola. The diagnosis is determined on the basis of its characteristic shape, localization and findings on optical coherence tomography (OCT). The etiology and pathogenesis of torpedo maculopathy is unclear, but it is believed to be a congenital defect of the retinal pigment epithelium (RPE). The aim of this publication is highlight this diagnosis and to present an incidental finding of torpedo maculopathy in an adult patient.
Case report: A 30-year-old female patient reported for a routine eye examination. Fundus examination of the right eye revealed an oval hypopigmented lesion with a size of 1 disk diameter inferotemporally from the fovea, which was followed by a satellite lesion in the same axis directed into the foveola. Based on OCT, OCT angiography, fundus autofluorescence, and the typical shape and location of the lesion, the patient was diagnosed with torpedo maculopathy in the right eye.
Conclusion: In general, torpedo maculopathy is an asymptomatic, congenital, benign retinal lesion, which is mostly diagnosed accidentally during a routine fundus examination. TM is non-progressive retinal finding with a minimal risk of deterioration of visual functions, which does not require any treatment. Nevertheless, due to the rare risk of a choroidal neovascular membrane, it is recommended to examine patients once a year. It is necessary to consider this diagnosis when a unilateral hypopigmented lesion is found inferotemporally from the fovea, and to distinguish it from chorioretinal atrophy, scar, vitelliform dystrophy, or other RPE lesions as part of the differential diagnosis.Keywords:
optical coherence tomography – macula – Retina – torpedo maculopathy – hypopigmented nevus
INTRODUCTION
Torpedo maculopathy (TM), also known as solitary hypopigmented nevus of the retinal pigment epithelium (RPE), paramacular albinotic spot syndrome or atypical macular coloboma, was first described by Roseman and Gass in 1992 [1]. The etiology and pathogenesis of TM is unclear, but it is assumed to be a congenital developmental defect of the RPE. The clinical picture is typically a unilateral, bordered, symmetrical, solitary hypopigmented lesion in the inferotemporal part of the macula. In most cases the lesion is located along the horizontal raphe, is oval in the shape of a torpedo, and the nasal edge is directed precisely into the foveola. The most commonly described size of the lesion is approximately 2 disk diameters (DD) horizontally and 1 DD vertically, usually without affecting the fovea [2–5]. Although TM is described as a solitary lesion in the macula, satellite lesions may appear, which are located temporally in a single line with the primary lesion. It mostly concerns a chance asymptomatic finding on the ocular fundus, which is stable and does not progress. Visual acuity is not affected, although microscotomas may appear in the visual field [2,4].
This is a relatively rare finding. In a review of TM it is stated that approximately 110 cases had been published up to 2021 [2]. With reference to its benign and asymptomatic character, the incidence, prevalence and demographics of TM are not known. Based on optical coherence tomography (OCT), Wong described two types of TM. In type 1 we detect a reduction of the outer layers of the neuroretina and RPE in the place of TM on OCT. This finding is very pathognomonic for TM. In type 2, in addition to this a cavitation (hyporeflective area) of the outer layers of the neuroretina and a dysfunction of the ellipsoid zone is displayed [6]. In 2018, Tripathy also described type 3, with focal choroidal excavation [7]. Wong assumes that these subtypes represent different stages of TM, which develop from type 1 to type 2 over the course of several decades [6].
1. Fundus photo (A) of the right eye with torpedo maculopathy, fundusautofluorescence (B) shows areas of hypofluorescence in the place of the main and satellite lesions, the red free image (C) highlighted the lesion 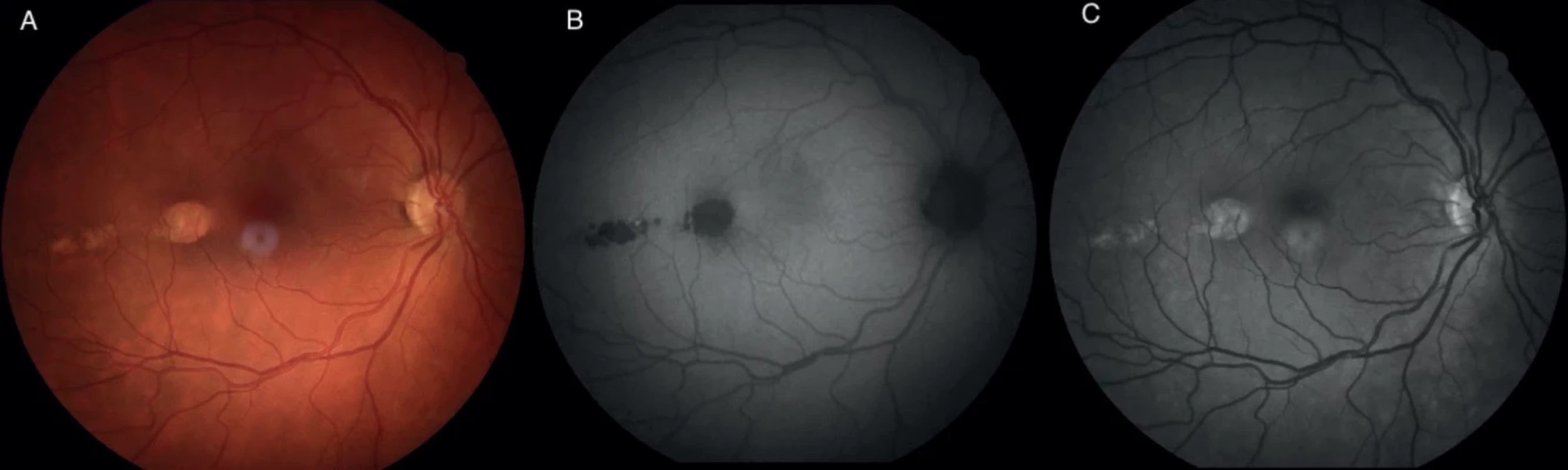
CASE REPORT
A 30-year-old female patient with mild myopia of -1.5 Dsf bilaterally reported to the emergency service of the Department of Ophthalmology at the University Hospital in Trenčín in March 2023 due to bilateral conjunctivitis and slight blurring of vision. Best corrected distance visual acuity was 1.0 in the right eye and 0.9 in the left eye. Bilateral superficial conjunctival injection and purulent secretion in the fornices was visible on the anterior segment, the other finding on the anterior segment was within the norm. An oval hypopigmented lesion with a size of 1 DD was visible on the ocular fundus, at a distance of approximately 1 DD inferotemporally from the fovea (Fig. 1). Satellite lesions were located in a single line temporally from the primary lesion, in the form of an atrophic-pigmented “tail”. The main and satellite lesions were directed in a single axis towards the foveola. We did not find similar lesions in the retinal periphery. The patient’s ocular, personal, working and pharmacological history was negative, and the patient had not suffered any ocular trauma in the past.
On fundus autofluorescence (FAF), areas of hypofluorescence are displayed in the area of the main and satellite lesion, correlating to damage to the RPE. The infrared and red-free image accentuated the contours of the lesion, which corresponds to the finding on the ocular fundus. On a horizontal transfoveal OCT scan of the macula, reduction is displayed in the outer nuclear layer, in the ellipsoid zone, the interdigital zone and the RPE layer (Fig. 2). OCT also demonstrated thinning and hyperreflectivity of the choroid beneath the lesion. On OCT we did not detect cavitation or choroidal excavation. The inner layers of the neuroretina, the region of the fovea and central retinal thickness were within the norm. On OCT angiography the superficial and deep capillary plexus had proportionate vascularity (Fig. 3). Due to RPE atrophy, the choriocapillaris layer had an increased signal. On a perimetric examination of the right eye, no abnormalities were shown in the visual field. Based on the shape, localization, medical history and OCT finding, we diagnosed the patient with TM, which corresponds to morphological OCT type 1. In the examinations of the left eye we did not find any lesion-related pathologies. The patient was treated with topical antibiotic eye drops for 7 days. At a follow-up examination after 2 weeks the patient stated no ocular complaints, and we are planning to monitor the patient once per year.
DISCUSSION
Torpedo maculopathy is a rare, benign retinal lesion. The typical finding is a unilateral hypopigmented lesion temporally from the fovea, with the tip directed towards the foveola [5]. Atypical forms of TM have also been described in the literature, as a bilateral finding, two torpedo-shaped lesions in one eye, a hyperpigmented TM lesion or a case of inferior TM with the tip oriented towards the optic nerve papilla [8,10]. TM is described as a solitary lesion, but satellite lesions may also appear, located in a single line with the primary lesion. All satellite lesions described to date are smaller and localized temporally [11]. TM is usually a chance finding in asymptomatic patients, it is of a non-progressing character and does not require any treatment. Visual functions are not usually affected, in rare cases patients describe microscotomas. To date, a total of 5 cases of appearance of a choroidal neovascular membrane (CNV) have been described within the terrain of TM [12]. Despite the fact that this is a rare complication, examination of the ocular fundus and OCT are recommended for patients with TM once per year.
The pathophysiology of origin of TM is unknown, and a number of theories have been pro-posed. Pian contends that the lesion could appear as a result of a developmental defect of the nerve fiber layers in the horizontal raphe [13]. Another hypothesis is that TM is a consequence of intrauterine chorioretinitis, or may concern abnormalities of the retinal or choroidal blood vessels [14]. Shields et al. consider the cause to be a defect in the development of the RPE in the socalled “temporal fetal bulge”. When Streeten studied the development of the RPE of the fetus, he noted that a cone-shaped bulge appears in the temporal region of the macula be-tween the 4th and 6th month of pregnancy, and this lesion gradually decreases in size between the 6th and 8th month. It is assumed that TM is a congenital defect of the RPE in the given point of development of the fetus [15]. To date no genetic analysis has confirmed an associa-tion between TM and mutation of a certain gene. Three analyzed genes (NEXMIF, TSC2, RP1L1) have been published, mutations of which have been confirmed in individuals with TM. However, these patients had affiliated systemic and ocular manifestations associated with mutation of the gene, and it is assumed that TM was a chance finding in these patients [16]. At present no evidence exists which could attest to an association between TM and other accompanying systemic or ocular pathologies [15].
Within differential diagnostics, TM resembles chorioretinal atrophy, scarring, coloboma, vitelliform dystrophy, congenital hypertrophy of the RPE or RPE lesion upon a background of Gardner syndrome [4]. Abnormalities of the RPE in combination with familial adenomatous polyposis in Gardner syndrome are similar to TM, but the lesions are smaller, pigmented, of irregular shape and with random localization on the retina. Congenital hypertrophy of the RPE is a flat congenital lesion of the RPE, which is mostly of more pronounced pigmentation, has rounded edges and is located on the periphery in different quadrants, but only rarely in the macula. Chorioretinal scarring is generally associated with a medical history of trauma, inflammatory process or wet form of age-related macular degeneration, and is displayed on OCT as hyperreflexive material. In contrast with TM, we can see translucent blood vessels in the place of chorioretinal atrophy, and on OCT we find more pronounced atrophic changes in all the layers of the retina and choroid. Best’s vitelliform macular dystrophy and its adult form has an image of an egg yolk in the center of the macula and a typical OCT finding [4].
2. OCT macular scan of the right eye shows a reduction in the outer retinal layers and RPE (red arrow), as well as hyperreflectivity and thinning of the choroid (white arrow) in the torpedo maculopathy lesion 
RPE – retinal pigment epithelium 3. OCT angiography of the right eye – the superficial and deep capillary plexus with normal vascularity and the choriocapillaris with an increased signal due to atrophy of RPE (white arrow) 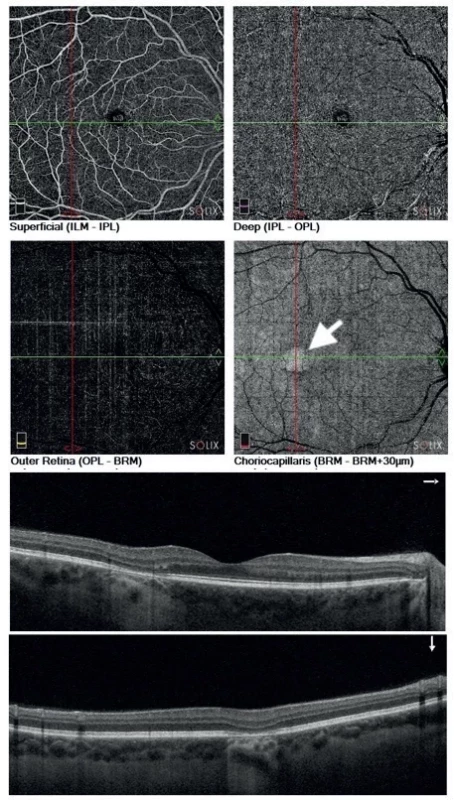
RPE – retinal pigment epithelium CONCLUSION
This study describes the case of a 30-year-old female patient with a chance finding of torpedo maculopathy in the right eye. Torpedo maculopathy is generally an asymptomatic, congenital, benign retinal lesion. In most cases it is diagnosed by chance upon an examination of the ocular fundus. It concerns a stable finding with a minimal risk of damage to visual functions, which does not require any treatment. Despite this, due to the rare risk of choroidal neovascular membrane, it is recommended that patients are monitored once per year and carry out self-examination with the aid of an Amsler grid. It is necessary to consider this rare diagnosis upon a finding of a unilateral hypopigmented lesion inferotemporally from the fovea, and within the framework of differential diagnostics to differentiate it from chorioretinal atrophy, scarring, coloboma, vitelliform dystrophy or other lesions of the RPE. Upon determination of the diagnosis, we consider the most important features to be the characteristic shape and localization of the lesion, negative medical history and OCT examination.
Sources
1. Roseman RL, Gass JD. Solitary hypopigmented nevus of the retinal pigment epithelium in the macula. Arch Ophthalmol. 1992;110 : 1762.
2. Menezes K, Mancera N, Patel H, Kattih Z, Mhaskar R. Torpedo Maculopathy: A Systematic Review of Case Reports. Ophthalmic Surg Lasers Imaging Retina. 2021;52(2):78-83.
3. Shirley K, O’Neill M, Gamble R, Ramsey A, McLoone E. Torpedo maculopathy: disease spectrum and associated choroidal neovascularization in a paediatric population. Eye. 2018;32 : 1315-1320.
4. Venkatesh R, Jain K, Pereira A, Thirumalesh, Yadav NK. Torpedo Retinopathy. J Ophthalmic Vis Res. 2020;15(2):187-194.
5. Yuan H, Dou H, Li X. Multimodal Imaging of Choroidal Structural in Torpedo Macu-lopathy. Front Med (Lausanne). 2023;10.
6. Wong EN, Fraser-Bell S, Hunyor AP, Chen FK. Novel optical coherence tomography classification of torpedo maculopathy. Clin Exp Ophthalmol. 2015;43 : 342-348.
7. Tripathy K, Sarma B, Mazumdar S. Commentary: Inner retinal excavation in torpedo maculopathy and proposed type 3 lesions in optical coherence tomography. Indian J Ophthalmol. 2018;66(8):1213-1214.
8. Smith MJ, Sia DIT, Greve M. Torpedo maculopathy-inferior variant. Can J Ophthal-mol. Published:March 18, 2021 (Article in press) doi:https://doi.org/10.1016/j.jcjo.2021.02.008
9. Richez F, Gueudry J, Brasseur G, Muraine M. Maculopathie en torpille bilatérale [Bilateral torpedo maculopathy]. J Fr Ophtalmol. 2010;33(4):296. French.
10. Ranjith PC, Giridhar, Anantharaman. Hyperpigmented torpedo maculopathy. Indian Journal of Ophthalmology. 2019;67(2):270-271.
11. Knani L, Werda S, Ghachem M, Mahjoub A. Multimodal imaging of torpedo maculopathy with optical coherence tomography angiography. Saudi J Ophthalmol. 2023;37(1):63-65.
12. Byer M, Rousso L, Rodman J, Shechtman D. Case Report: Use of Multimodal Imaging to Document a Rare Complication of Torpedo Maculopathy. Optom Vis Sci. 2021;98(8):870-875.
13. Pian D, Ferrucci S, Anderson SF, Wu C. Paramacular coloboma. Optom Vis Sci. 2003;80 : 556-563.
14. Papastefanou VP, Vázquez-Alfageme C, Keane PA, Sagoo MS. Multimodality imaginf of torpedo maculopathy with swptsource, en face optical coherence tomography and optical coherence tomography angiography. Retin Cases Brief Rep. 2018;12(2):153-157.
15. Shields CL, Guzman JM, Shapiro MJ, Fogel LE, Shields JA. Torpedo Maculopathy at the Site of the Fetal “Bulge”. Arch Ophthalmol. 2010;128(4):499-501.
16. Soman J, Sheth JU, Indurkar A, Nair U. Torpedo Maculopathy Associated with RP1L1 Mutation and Rod-Cone Dystrophy. Acta Scientific Ophthalmology. 2021;138-141.Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2023 Issue 5-
All articles in this issue
- Úvod do Doporučených postupů
- XXXI. Výroční sjezd ČOS. Anonce
- Vzpomínka na doc. Hejcmanovou. Nekrolog
- Doporučené postupy diagnostiky a léčby diabetického makulárního edému
- Doporučené postupy diagnostiky a léčby diabetické retinopatie
- Screening diabetické retinopatie a diabetického makulárního edému
- Využitie rohovkovej topografie v detskej oftalmológii
- Torpédo makulopatia. Kazuistika
- Determination of Corneal Power after Refractive Surgery with Excimer Laser: A Concise Review
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Doporučené postupy diagnostiky a léčby diabetického makulárního edému
- Doporučené postupy diagnostiky a léčby diabetické retinopatie
- Screening diabetické retinopatie a diabetického makulárního edému
- Torpédo makulopatia. Kazuistika
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

