-
Medical journals
- Career
Harmonic scalpel versus traditional ligation in axillary dissection for breast cancer: a retrospective multivariate analysis
Authors: J. Zatecky 1,2; O. Kubala 1,3; P. Jelínek 1,3; M. Lerch 2; P. Ihnát 1,3; M. Peteja 1,2; R. Brát 1
Authors‘ workplace: Katedra chirurgických oborů, Lékařská fakulta, Ostravská univerzita 1; Chirurgické oddělení, Slezská nemocnice v Opavě 2; Chirurgická klinika, Fakultní nemocnice Ostrava 3
Published in: Rozhl. Chir., 2020, roč. 99, č. 11, s. 502-508.
Category: Original articles
Overview
Introduction: The aim of this pilot retrospective study is to evaluate the complication rate in patients after axillary dissection comparing preparation with harmonic scalpel vs traditional ligation technique, and to analyse risk factors for complications occurrence.
Methods: 144 patients with 148 axillary dissections operated in a single centre between January 2014 and 2019 were included into the study. Axillary dissection was performed using harmonic scalpel in 73 and absorbable ligations in 70 cases.
Results: Seroma formation was observed in 41 patients (56.2%) in the harmonic scalpel group and in 21 patients (30.0%) in the ligations group (p=0.003). The mean period from the surgery to drain removal was 4.0 days in the harmonic scalpel group and 3.0 days in the ligations group (p<0.001). The mean amount of the drained fluid after mastectomy was 300.9 ml in the harmonic scalpel group and 168.7 ml in the ligations group (p=0.005); after breast conserving surgery, it was 241.9 ml and 107.4 ml, respectively (p =0.023).
Conclusion: In comparison with traditional ligations with absorbable material, axillary dissection using harmonic scalpel significantly increases the risk of postoperative seroma formation, prolongs the time from the surgery to drain removal, and increases the amount of drained fluid.
Keywords:
breast cancer − axillary dissection – ligation − harmonic scalpel − seroma
Introduction
Breast cancer is the most common type of cancer in women affecting annually 2.1 million women worldwide [1]. The development of surgical procedures in breast cancer surgery over the last decades has led to reduction of radicality in the surgical management of breast tumours as well as of axillae – from mastectomy with axillary dissection usually indicated in the past the to possibility of performing segmentectomy or tumorectomy with sentinel lymph node biopsy.
Patients profit from this lower radicality by reduction of postoperative morbidity (e.g. lymphoedema, neuralgia, wound complications etc.) with the same mortality rate [2]. Despite these facts, axillary dissection still remains a common method for axillary management in a well-selected group of patients.
The aim of our study was to evaluate the complication rate in patients with breast cancer after axillary dissection and to compare two methods of preparation – harmonic scalpel and traditional ligation.
Methods
The study was designed as a clinical retrospective single-centre trial. The study protocol was approved by the local ethics committee and by the ethics committee of the Faculty of Medicine, University of Ostrava. All patients with breast cancer confirmed by biopsy operated in the Department of Surgery, Silesian hospital in Opava between 1. 1. 2014 and 1. 1. 2019 in whom axillary dissection was performed were included into study. Exclusion criteria were a lack of information due to no follow-up or previous disagreement with participation in any study.
Patients were operated by skilled breast surgeons who performed either breast conserving surgery (BCS) or mastectomy (MAE) with or without sentinel lymph node biopsy (SLNB). In all patients included in the study, axillary lymph node dissection (ALND) of level I and II was performed according to the recommendation of multidisciplinary team. When the SLNB was part of an operation, the decision to perform the ALND was made immediately during the same operation.
Axillary lymph node dissection was performed using one of three methods, the most common of which were the dissection/coagulation with harmonic scalpel or tissue preparation using ligation with absorbable material for closing lymphatic and blood vessels. A few patients were operated by electrocautery, but due to the small number, they were not included into the statistical analysis of complications.
Recorded patient characteristics included the age, BMI, tumour type, duration and type of the surgery (BCS, MAE, SLNB, ALND), the surgical technique during ALND, complications, neoadjuvant chemotherapy and the number of lymph nodes.
After the surgery, Redon drain was applied in each patient; the number of days from the operation to the drain removal and amount of the drained fluid were recorded. The drains were removed when the volume of fluid was below 30 ml/24 hour. Two patients were excluded from this analysis because of drain malposition and fluid leakage around the drain.
The primary outcome was to observe the relationship between the surgical technique in ALND (harmonic scalpel or ligations) and postoperative complications, mainly seromas. The secondary outcome was to analyse the potential risk factors for development of postoperative complications.
The multivariate statistical analysis of the dataset was performed in the software R 3.4.3 with the packages „sciplot“, „MASS“, „lme4“, „MuMIn“ and „car“. Values in Results are shown in the format of mean ± standard error of mean. The p-values were calculated using Pearson‘s Chi-squared test with Yates’s continuity correction and the results were considered as statistically significant if p<0.05.
Results
144 patients meeting the criteria were included into the study; in 4 patients, bilateral breast surgery with axillary dissection was performed, which led to a total of 148 axillary dissections. The mean age of patients was 65.4 years, median 67 years, with a minimum of 34 and maximum of 88 years. The number of lymph nodes harvested during ALND varied between minimum of 2 and maximum of 27 with mean number 10.5 and median 10. Histologically, the most common type of breast cancer was a ductal carcinoma in 109 cases (73.7%), the second most common was the lobular carcinoma in 26 cases (17.6%). The TNM classifications of patients in the individual groups is detailed in Tab. 1. No significant difference between groups was detected in any of the parameters. The complications listed below was Clavien-Dindo grade I only, no serious complication occured and no reoperation was necessary.
1. The number of axillary dissections according to the TNM classification, histological findings and the method of ALND
(No significant difference between groups was detected in any of the parameters) Harmonic scalpel Ligation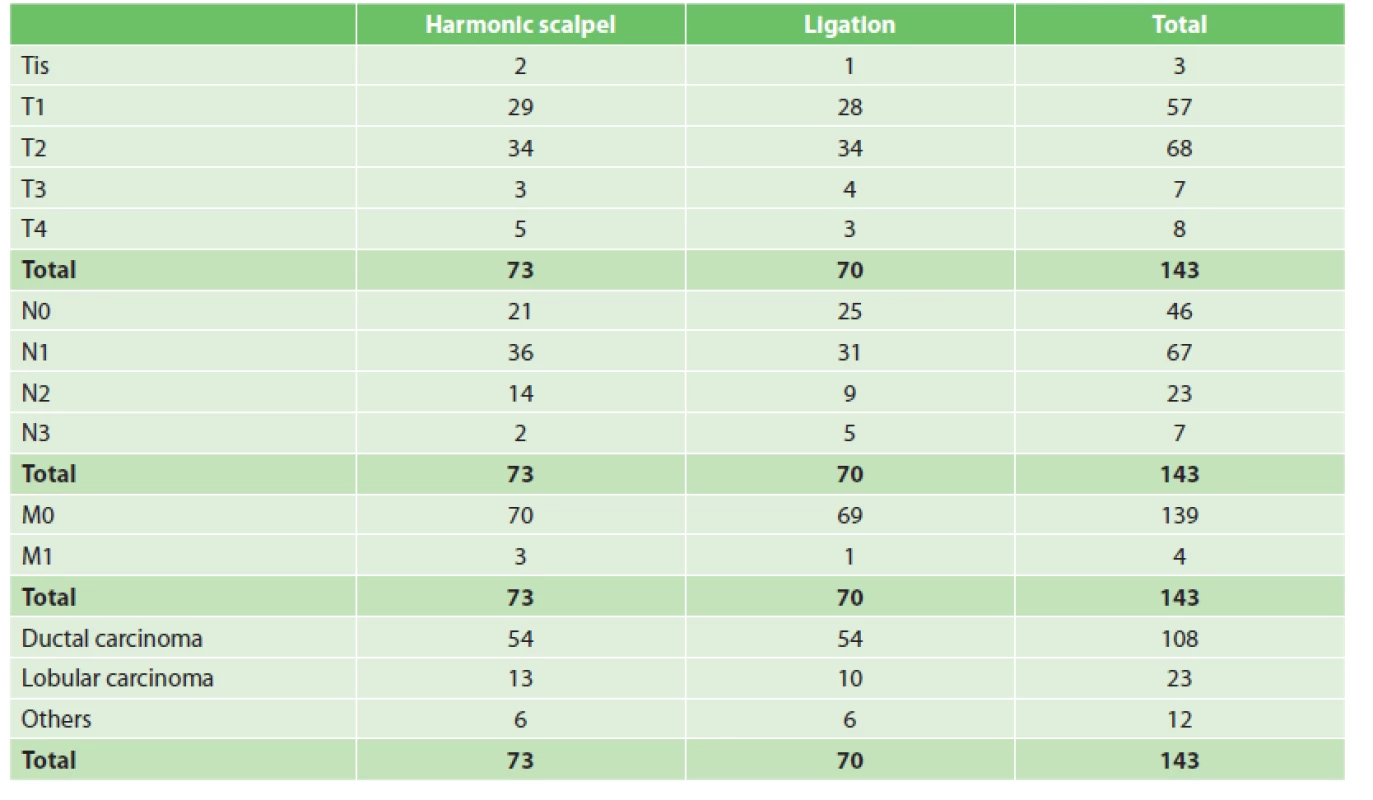
The axillary dissection was performed using harmonic scalpel in 73 patients, using absorbable ligations in 70 patients and using electrocautery in 5 patients (who were not included in statistical analysis due to the small number of patients). The numbers of patients undergoing individual types of surgery is shown in Tab. 1. Seroma formation was observed in 41 patients (56.2%) in the harmonic scalpel group and in 21 patients (30.0%) in the ligation group (Fig. 1), yielding statistically significant difference between the harmonic scalpel and ligations group (p=0.003, χ2=8.92).
1. The relationship between the methods of axillary dissection and postoperative seroma occurrence 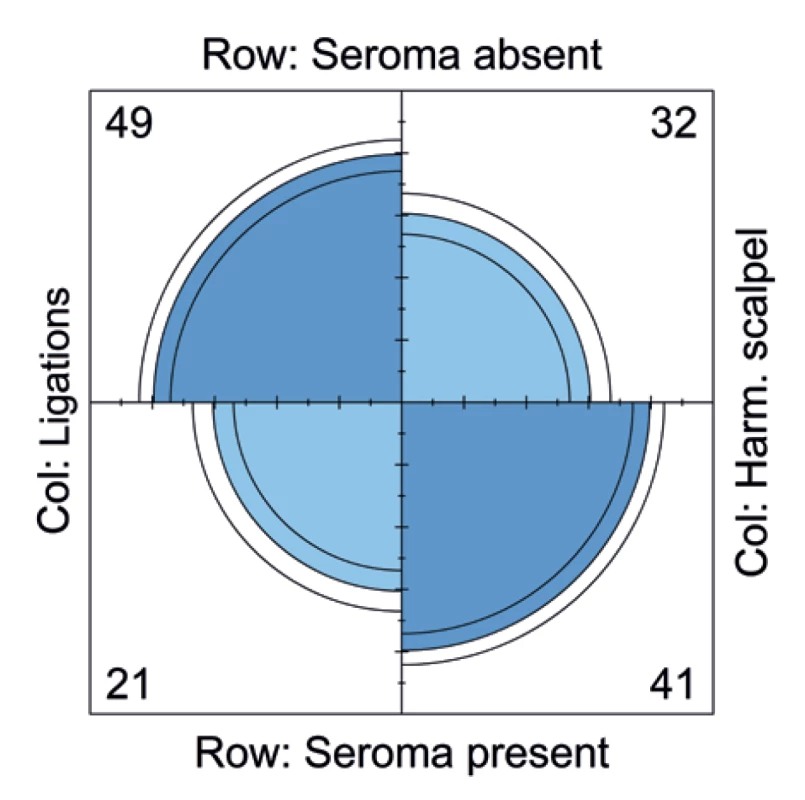
Association of two other complications – lymphoedema and inflammatory complications –with the method of axillary dissection was also evaluated. No significant difference was observed in the development of postoperative lymphoedema (p=0.535, χ2=0.38; Fig. 2) or inflammatory complications (p=0.711, χ2=0.13; Fig. 3) between the two surgical techniques.
2. The relationship between the method of axillary dissection and postoperative lymphoedema 
3. The relationship between the method of axillary dissection and inflammatory complications 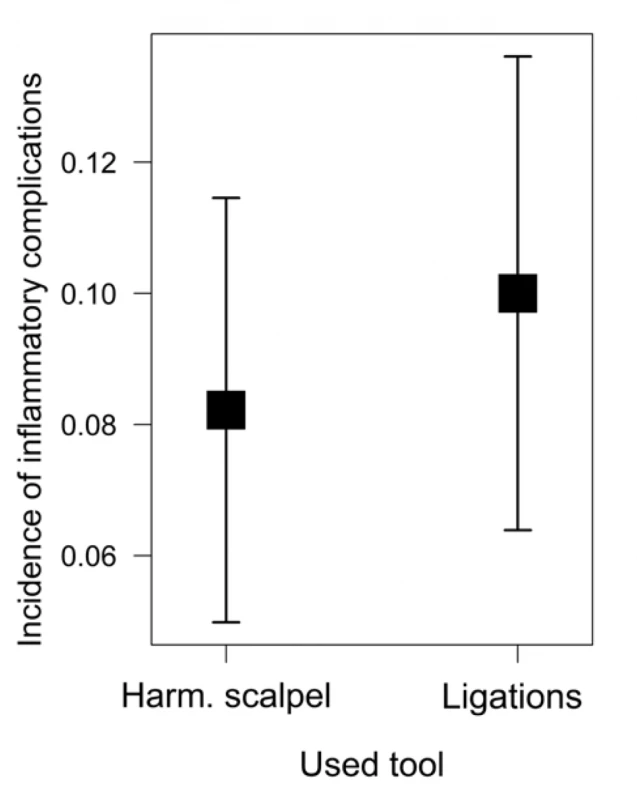
The time from the surgery to drain removal as well as the amount of the drained fluid were also recorded. The mean time from operation to drain removal was 4.0 (±0.18) days in the harmonic scalpel group and 3.0 (±0.14) days in the ligation group, which was highly significant (p< 0.001, χ2=15.47; Fig. 4). To avoid any bias associated with different operations, the patients were further divided into the mastectomy and breast-conserving surgery groups. The mean time from operation to drain removal after mastectomy was 4.1 (±0.22) days in the harmonic scalpel group and 3.0 (±0.16) days in the ligations group (p=0.004, χ2=8.32); after breast conserving surgery, the mean period was 3.8 (±0.32) days in the harmonic scalpel group and 2.9 (±0.31) days in the ligations group (p=0.114, χ2=2.49). Here, it is however necessary to note that the insignificant result might have been influenced by a small total number of patients with breast conserving surgery (n=40).
4. The relationship between the method of axillary dissection and the mean time from operation to drain removal 
The mean total amount of drained fluid from the operation to drain-removal after mastectomy was 296.0 (±27.36) ml in the harmonic scalpel group and 168.7 (±22.02) ml in the ligations group; after breast conserving surgery, it was 241.9 (±38.26) ml in the harmonic scalpel group and 107.4 (±31.31) ml in the ligations group. Again, results were statistically highly significant (p=0.005/0.023, χ2=8.05/5.16; Fig. 5).
5. The relationship between the method of axillary dissection and the mean amount of drained fluid 
The operation time was also analysed according to the type of surgery and surgical technique. The surgery duration was statistically significantly longer for the ligation than for harmonic scalpel technique in mastectomy both with/without SLNB (p=0.002/0.039, χ2=12.42/4.41); this difference was however not significant in BCS, neither with (p=0.074, χ2=0.96) nor without SLNB (p=0.537, χ2=3.40; See Fig. 6). Here again, it is however necessary to take into account the number of patients in the BCS group and subgroups (see Tab. 2).
2. The number of axillary dissections in individual subgroups according to the type of operation and the method of ALND 
6. The relationship between the method of axillary dissection, the type of operation and surgery duration 
In multivariate analysis, we focused on identifying factors possibly associated with complications. 9 patients with neoadjuvant chemotherapy (NAC) were present in the study group. Statistically, no associations between NAC and complications rate was observed (p=0.327, χ2=0.96), which however can be associated with the error caused by small numbers.
Association between the age and complication rate was also analysed. Age alone had no influence on the occurrence of complications (p=0.814, χ2=0.06). However, when analysing individual subgroups, statistically significant relationships were identified. In the group with ALND operated using harmonic scalpel, the complication rate grew with increasing age while in the group operated using ligation technique, it was slightly decreasing (p=0.008, χ2=9.70; Fig. 7).
7. The relationship between the complication rate, age and the method of axillary dissection 
The relationship of body weight (represented by body-mass index, BMI) to developing complications was also analysed with a borderline insignificant result (p=0.068, χ2=3.33; Fig. 8).
8. The relationship between the complication rate and BMI 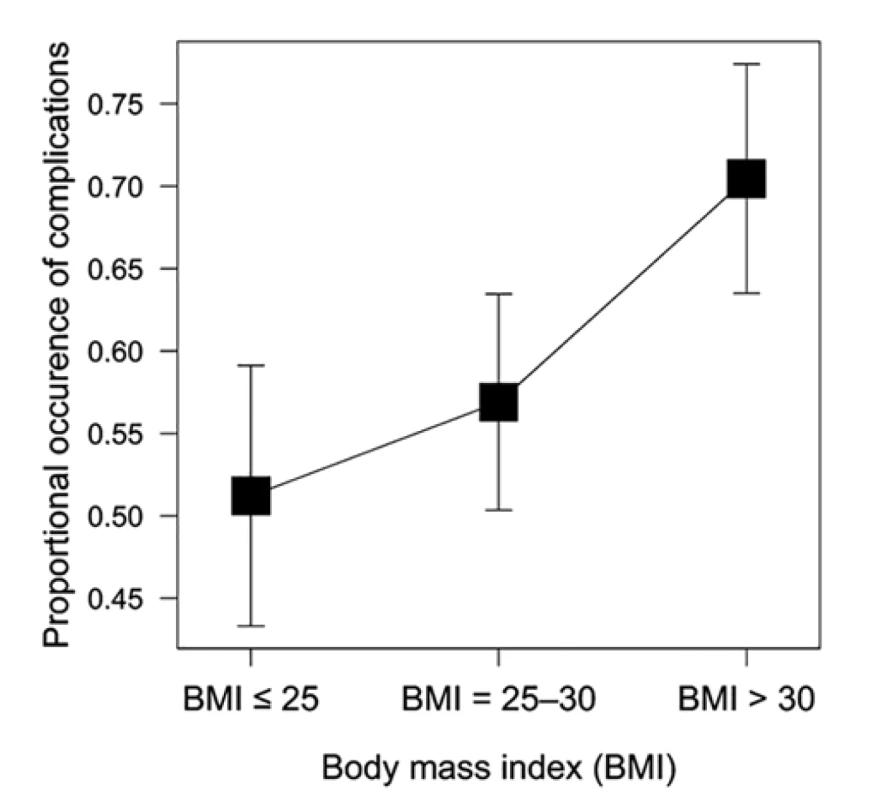
The analysis of the relationship between the number of lymph nodes infiltrated by tumour cells after axillary dissection and complications rate was also performed. We found out that although the complication rate was increasing with the growing number of tumour-infiltrated lymph nodes, the result was (albeit closely) not statistically significant (p=0.066, χ2=3.37; Fig. 9).
9. The relationship between the complication rate and the number of tumour-infiltrated lymph nodes 
Discussion
Seroma formation is the most common complication arising after breast cancer surgery; according to various authors, its occurrence is between 2.5 % to 90 % [3,4]. In our study, the occurrence was 43.36 %. Postoperative seroma can complicate wound healing, prolong hospitalisation, increase the number of follow-ups after the surgery, complicate the initiation of the adjuvant treatment and result in significant patient’s discomfort. Some authors consider seroma not as a complication, but rather as a sequel to [4,5] or an inevitable consequence [6] of breast cancer surgery. According to our results, we can’t completely agree. Statistically significantly higher occurrence of seroma in the harmonic scalpel (56.2%) versus ligation group (30.0%) and the longer time from the surgery to drain removal along with the higher amount of drained fluid means that the development of seroma is far from inevitable and that surgical technique is one of the significant factors influencing the incidence of seroma. The pathogenesis of seroma formation has not yet been fully explained; some authors believe that multiple mechanisms are involved, such as acute inflammatory response, leakage from lymphatic vessels, tissue devascularization, or thermal trauma with lipolysis caused by electrosurgical sealing systems [7].
Many studies comparing methods for axillary dissection in view of reducing seroma formation have been published but no trial compared the use of harmonic scalpel and traditional ligation with absorbable material as in our research; hence, we can consider our trial as a pilot study.
Most published studies compare harmonic scalpel and monopolar electrocautery techniques with inconclusive results [6]. Some published trials support the use of harmonic scalpel [7,8,9,10,11], some of them however found it more expensive and resulting in the same seroma rate as electrocautery [12,13,14,15,16]. Three meta-analyses were published on this topic, but again, the results are inconsistent [17,18,19]. Cheng et al. published a meta-analysis proving that harmonic scalpel reduces complications by about half compared with electrocautery [17]; Huang et al. found that the harmonic technology presented advantages in reducing postoperative drainage, seroma development, intraoperative blood loss and wound complications [18]; the meta-analysis by Currie et al. however reported similar results for both – harmonic scalpel and electrocautery [19].
Nadkarni et al. compared the electrocautery and traditional ligatures, observing that the surgical technique had no effect on seroma formation in breast cancer surgery [3]; on the other hand, Chavan et al. clearly concluded that the use of electrocautery should be restricted during mastectomy and axillary dissection because of significantly higher seroma formation rate [20].
According to the study published by Nespoli et al., bipolar vessel sealing system (BVSS) offers only marginal advantages over monopolar electrocautery and the seroma incidence was similar in both groups [21]. A meta-analysis performed by Pergialiotis et al. concluded that BVSS increases the accuracy of axillary dissection and is a safe method compared to ligation, even though BVSS increases incidence of seroma rate [22].
All current methods for axillary dissection are associated with some complications; the results from clinical trials and meta-analyses do not clearly recommend any one of them over the others. An ideal method for axillary dissection is still to be developed [16].
Other risk factors for the occurrence of complications in our study included the higher age in harmonic scalpel axillary dissection; BMI over 30 and higher number of lymph nodes involved by tumour, which are also mentioned in study by Nespoli et al. [21], were in our study borderline insignificant so although we cannot confirm this hypothesis, there is a clear tendency towards such a result. Other risk factors for seroma and lymphorrhea development according to the literature are the tumour size, extent of gland resection and neoadjuvant chemotherapy [21]. Results of studies examining the complication rate after neoadjuvant chemotherapy are also mixed. Xue et al. published a meta-analysis with multivariate analysis of many risk factors and did not find preoperative chemotherapy as a statistically significant risk factor [23]; similarly, Bowen et al. reported no increase in the risk of surgical morbidity in patients after neoadjuvant treatment following mastectomy [24]. On the other hand, Garvey et al. concluded that surgery after NAC is safe but major complications should be expected, especially in patients with immediate reconstruction of the breast [25].
Thanks to the progress in breast cancer surgery, criteria for performing axillary dissection are getting more and more strict and ALND is often substituted with other methods such as sentinel lymph node biopsy. Patients’ benefit from SLNB include the lower surgical morbidity such as seromas, lymphoedema and neuralgia of the operated limb. New challenges associated with neoadjuvant therapy usage arise, new methods are being developed. Targeted axillary dissection, which is a combination of SLNB and biopsy of pathological lymph nodes, is a promising method of axillary staging, which can replace axillary dissection of level I and II in selected patients, but it is highly dependent on the use of a reliable marker [26].
Conclusion
In comparison with traditional ligation with absorbable material, axillary dissection using harmonic scalpel significantly increases the risk of postoperative seroma formation, prolongs time from operation to drain removal, increases the amount of drained fluid and shortens the operation time in mastectomy associated with ALND both with and without SLNB. Age was a significant risk factor after harmonic scalpel usage, BMI and number of lymph nodes involved with tumour showed a tendency to be risk factors, they were however borderline insignificant. Our findings are nevertheless yet to be confirmed by a prospective study.
Ethical approval
The research was approved by the Ethics Committee of Faculty of Medicine, University of Ostrava (EK 20/2019) and the Ethics Committee of the Silesian Hospital in Opava (EK SNO 332/2019).
The study was supported by the Student Grant Competition of Specific University Research of the University of Ostrava (SGS04 / LF / 2018-2019).
Conflict of interests
The authors declare that they have no conflict of interest in connection with this paper and that the article was not published in any other journal except congress abstracts and clinical guidelines.
MUDr. Jan Žatecký
Slezská 233
Neplachovice
Czech Republic
ORCID: 0000-0002-0415-0853
e-mail: jan.zatecky@snopava.cz
Sources
- WHO | Breast cancer [On-line] WHO. [cited 2019 Aug 15]. Available from: http://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/.
- NCCN Guidelines Insights: Breast Cancer, Version 3.2018 in: Journal of the National Comprehensive Cancer Network 2019;17(2). doi: https://doi.org/10.6004/jnccn.2019.0009.
- Anand R, Skinner R, Dennison G, et al. A prospective randomised trial of two treatments for wound seroma after breast surgery. Eur J Surg Oncol. 2002;28(6):620−622. doi: 10.1053/ejso.2002.1298
- Nadkarni MS, Rangole AK, Sharma RK, et al. Influence of surgical technique on axillary seroma formation: a randomized study. ANZ J Surg. 2007;77(5):385−389. doi:10.1111/j.1445-2197.2007.04067.x.
- Agrawal A, Ayantunde AA, Cheung KL. Concepts of seroma formation and prevention in breast cancer surgery. ANZ J Surg. 2006;76(12):1088−1095. doi:10.1111/j.1445-2197.2006.03949.x.
- Wyld L, Markopoulos C, Leidenius M, et al. Breast cancer management for surgeons: A European multidisciplinary textbook. Springer International Publishing 2018.
- Iovino F, Auriemma PP, Ferraraccio F, et al. Preventing seroma formation after axillary dissection for breast cancer: a randomized clinical trial. Am J Surg. 2012;203(6):708−714. doi:10.1016/j.amjsurg.2011.06.051.
- Böhm D, Kubitza A, Lebrecht A, et al. Prospective randomized comparison of conventional instruments and the Harmonic Focus® device in breast-conserving therapy for primary breast cancer. European Journal of Surgical Oncology (EJSO). 2012;38(2):118−124. doi:10.1016/j.ejso.2011.11.003.
- Rohaizak M, Khan FJ, Jasmin JS, et al. Ultracision versus electrocautery in performing modified radical mastectomy and axillary lymph node dissection for breast cancer: a prospective randomized control trial. Med J Malaysia 2013;68(3):204−207.
- Hung SH, Chu D, Chen FM, et al. Evaluation of the harmonic scalpel in breast conserving and axillary staging surgery. Journal of the Chinese Medical Association 2012;75(10):519−523. doi:10.1016/j.jcma.2012.07.006.
- Archana A, Sureshkumar S, Vijayakumar C, et al. Comparing the harmonic scalpel with electrocautery in reducing postoperative flap necrosis and seroma formation after modified radical mastectomy in carcinoma breast patients: A double-blind prospective randomized control trail. Cureus 2018;10(4):e2476. doi:10.7759/cureus.2476.
- Galatius H, Okholm M, Hoffmann J. Mastectomy using ultrasonic dissection: effect on seroma formation. The Breast 2003;12(5):338−341. doi:10.1016/S0960-9776(03)00110-3.
- He Q, Zhuang D, Zheng L, et al. Harmonic focus versus electrocautery in axillary lymph node dissection for breast cancer: A randomized clinical study. Clinical Breast Cancer 2012;12(6):454−458. doi:10.1016/j.clbc.2012.07.014.
- Ribeiro GHFP, Kerr LM, Haikel RL, et al. Modified radical mastectomy: a pilot clinical trial comparing the use of conventional electric scalpel and harmonic scalpel. Int J Surg. 2013;11(6):496−500. doi:10.1016/j.ijsu.2013.03.013.
- Deo SVS, Shukla NK, Asthana S, et al. A comparative study of modified radical mastectomy using harmonic scalpel and electrocautery. Singapore Med J. 2002;43(5):226−228.
- Isozaki H, Yamamoto Y, Murakami S, et al. Impact of the surgical modality for axillary lymph node dissection on postoperative drainage and seroma formation after total mastectomy. Patient Saf Surg. 2019;13 : 20. doi:10.1186/s13037-019-0199-z.
- Cheng H, Clymer JW, Ferko NC, et al. A systematic review and meta-analysis of Harmonic technology compared with conventional techniques in mastectomy and breast-conserving surgery with lymphadenectomy for breast cancer. Breast Cancer (Dove Med Press) 2016;8 : 125−140. doi:10.2147/BCTT.S110461.
- Huang J, Yu Y, Wei C, et al. Harmonic scalpel versus electrocautery dissection in modified radical mastectomy for breast cancer: A meta-analysis. PLoS ONE 2015;10(11):e0142271. doi:10.1371/journal.pone.0142271.
- Currie A, Chong K, Davies GL, et al. Ultrasonic dissection versus electrocautery in mastectomy for breast cancer - a meta-analysis. Eur J Surg Oncol. 2012;38(10):897−901. doi:10.1016/j.ejso.2012.05.006.
- Chavan RN, Chikkala B, Mondal P, et al. Comparison study between scalpel and electrocautery, in causation of seroma after modified radical mastectomy. Indian J Surg. 2017;79(5):423−426. doi:10.1007/s12262-016-1501-2.
- Nespoli L, Antolini L, Stucchi C, et al. Axillary lymphadenectomy for breast cancer. A randomized controlled trial comparing a bipolar vessel sealing system to the conventional technique. Breast 2012;21(6):739−745. doi:10.1016/j.breast.2012.08.003.
- Pergialiotis V, Kontzoglou K, Dimitroulis D, et al. Electrosurgical bipolar vessel sealing during axillary lymphadenectomy: a systematic review and meta-analysis. Breast Dis. 2015;35(1):5−11. doi:10.3233/BD-140383.
- Xue DQ, Qian C, Yang L, et al. Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol. 2012;38(5):375−381. doi:10.1016/j.ejso.2012.02.179.
- Bowen ME, Mone MC, Buys SS, et al. Surgical outcomes for mastectomy patients receiving neoadjuvant chemotherapy: A propensity-matched analysis. Ann Surg. 2017;265(3):448−456. doi:10.1097/SLA.0000000000001804
- Garvey EM, Gray RJ, Wasif N, et al. Neoadjuvant therapy and breast cancer surgery: a closer look at postoperative complications. Am J Surg. 2013;206(6):894−898; discussion 898−899. doi:10.1016/j.amjsurg.2013.09.004.
- Žatecký J, Kubala O, Jelínek P, et al. (in press) Magnetic marker localisation in breast cancer surgery. Archives of Medical Science 2020. doi:10.5114/aoms.2020.93673.
Labels
Surgery Orthopaedics Trauma surgery
Article was published inPerspectives in Surgery

2020 Issue 11-
All articles in this issue
- History of thyroid surgery
- What should a surgeon known about genetic background of thyroid cancer
- Papillary thyroid microcarcinoma and papillary thyreoid cancer at the Department of Surgery, EUC Clinic Zlín
- Retrosternal goiter
- Differentiated thyroid microcarcinoma − current perspective
- Harmonic scalpel versus traditional ligation in axillary dissection for breast cancer: a retrospective multivariate analysis
- Endoscopic approaches in head and neck endocrine surgery − introduction of TOETVA (TransOral Endoscopic Thyroidectomy by Vestibular Approach) into clinical use at the Department of Surgery of the University Hospital in Brno
- Chirurgie štítné žlázy a příštítných tělísek
- Zakladatel německé neurochirurgie a prvního samostatného neurochirurgického časopisu Wilhelm Tönnis (1898–1978) – dílo v kontextu doby
- Perspectives in Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Retrosternal goiter
- History of thyroid surgery
- Papillary thyroid microcarcinoma and papillary thyreoid cancer at the Department of Surgery, EUC Clinic Zlín
- What should a surgeon known about genetic background of thyroid cancer
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

