-
Medical journals
- Career
The impact of shift work on sleep and anxiety in general nurses
Authors: Š. Vévodová 1; B. Petrášová 2; J. Vévoda 1; A. Boriková 3; M. Nakládalová 3
Authors‘ workplace: Ústav společenských a humanitních věd, Fakulta zdravotnických věd, Univerzita Palackého v Olomouci přednostka Mgr. Šárka Vévodová, Ph. D. 1; Střední zdravotnická škola a Vyšší odborná škola zdravotnická Emanuela Pöttinga, Olomouc ředitel Mgr. Pavel Skula 2; Klinika pracovního lékařství Lékařské fakulty Univerzity Palackého v Olomouci přednostka doc. MUDr. Marie Nakládalová, Ph. D. 3
Published in: Pracov. Lék., 68, 2016, No. 3, s. 103-109.
Category: Original Papers
Overview
Introduction:
Shift work is inherently related to the healthcare work system because only then is it possible to ensure continuous work of this public service. At the same time, the shift work means intervention in the natural human bio-rhythms. The aim of this research was to investigate the impact of the shift work on sleep and anxiety in general nurses.Material and methods:
The quantitative research was realized by means of Pittsburgh Sleep Quality Index and Beck anxiety inventory questionnaires. In 2016, 100 nurses working in single shifts and 100 general nurses in combined shift were addressed in three healthcare in-patient providers (by random selection) in the Olomouc region. The return rate of the questionnaires was 60.5%. Out of 121 returned questionnaires, 56 general nurses in single shift work were aged 40.77 (SD = 9.44) with length of work experience 20.70 years (SD = 10.05); and 65 general nurses working in combined shift work and morning shifts with the average age 38.29 (SD = 9.36) and work experience length 17.57 years (SD = 8.97). For the data processing, Mann-Whitney test at 5% significance level and Spearman’s rank correlation coefficient at significance level of 5% and 1% respectively were used.Results:
The average sleep duration in general nurses working in shifts was 6.49 hours and the average sleep duration in general nurses working only morning shifts was 6.88 hours. The results of the research indicate that the group of general nurses working in shifts has a significantly higher rate of sleep disorders (p < 0.01) and a higher rate of anxiety symptoms (p = 0.04) compared to the control group. It has been ascertained with a higher rate of sleep disorders, the anxiety level in general nurses increases (rs = 0.596 (p ≤ 0.01). The results of the research reveal the existence of a link between rate of anxiety symptoms and daytime dysfunction rate (rs = 0.337 (p ≤ 0.01). The results have not confirmed a relation between the length of work experience of respondents and sleep disturbance rate or anxiety symptoms.Conclusion:
It is vital to support sleep hygiene and biorhythms in general nurses as much as possible.Key words:
nurse – lifestyle – shift work – sleep – sleep quality – anxietyINTRODUCTION
Professional life is one of the most frequent reasons for the unmet need for natural human sleep. Nowadays, people sleep 1–2 hours less than their naturally need for professional reasons [2]. There is a decreasing tendency in the number of subjects sleeping longer than 8 hours and vice versa, there is a rising tendency in the number of subjects sleeping less than 5 hours [2]. Shift work is one of the basic conditions for meaningful functioning of healthcare as a continuous public care and service [1]. But at the same time, it represents one of the stress factors in general nurse profession [3]. Sleep is often negatively influenced amongst general nurses both by regular biorhythm disruption caused by early waking-up for morning--shift and a disruption of whole circadian rhythm in shift work [6].
Sleep deprivation
Sleep debt gradually changes to sleep deprivation, which negatively influences the quality of one’s life, work efficiency and error rate. Sleep deprivation subsequently leads to psychic pro-blems among which anxiety plays a significant role [13] because it correlates with sleep disorders [18]. Sleep disorders are followed by neurotic and anxiety disorders regularly in up to 41% of cases [18]. Nurses diagnosed with generalized anxiety disorder suffer from sleep disorders and falling asleep difficulties most frequently [11]. More than one third of the world population suffers from insomnia. Of the total number of all insomnia types there are about 40–60% associated with depressive or anxiety disorder (including primary insomnia and sleeplessness accompanied by respiratory and movement disorders) [19, 30]. A significant positive correlation between shift work and anxiety symptoms in the general nurses was proven [9].
The fatigue caused by secondary sleep disorders is one of the significant contributors to the error rate in health care [23]. In these individuals, the increased error rate is mostly due to daytime dysfunction e.g. uncontrolable urge to sleep, sudden concentration and orientation loss [28]. The above mentioned disorders can pose a great risk for every health care provider and therefore they are a problem not only on psychological and medical at the individual level but ultimately also bectecome a system issue from the economical (solution and compensation for the loss suffered) and legal (forced judicial treatment of possible serious misconduct) point of view.
In terms of the health protection and occupational safety, these symptoms must not be underestimated as they may lead to an emergency inception. Lapse in attention, slowed reactions, movement coordination decrease, short-term failures or deteriorated information processing are among the most common symptoms of deteriorated cognitive performance [2, 4, 5, 6, 21]. Solution to this problem requires cooperation of health care providers’ management with their employees. Management should try to accommodate the employees and together they should set shift work they find most suitable [16]. Sleep deprivation manifests itself also by an increased systolic pressure, increase of cortisol, palpitation, tremor, itching, burning, eye redness and lower body temperature [17]. There is an individual tolerance regarding sleep deprivation. There is a universal negative tolerance of long-term suffering from insufficient sleep [6].
Shift work as a reason for circadian rhythm disorders
Shift work can be organized in various ways but it inherently brings a significant interference into natural biorhythms of a human organism [4]. Shift work interferes with sleep primarily by the fact that a day sleep is not an adequate compensation of a night sleep neither in terms of quality, nor duration [6]. Regular night sleep omission leads to chronic sleep restriction. When getting through the night shift, there is usually sleep reduction of 3–4 hours within the next 24 hours [2, 11]. Such an acute sleep deprivation, if sporadic, could be naturally compensated in the long run, but that is impossible in regular shift work. The most common consequences of sleep deprivation are sleepiness, concentration and memory disorders, reduction in alertness, indigestion and last but not least hypno-tics or alcohol abuse and tendency to injuries [4]. The circadian cycle disorder becomes substantial as early as after a month of sleep deprivation caused by shift work [5].
Physiological factors influencing sleep quality of people performing shift work are connected to natural organism setting for light-dark cycles [10]. Quality of sleep is fundamentally influenced by the hormone melatonin produced in the pineal gland. Its production is stimulated by darkness and inhibited by light [6, 26]. Currently, melatonin is used against insomnia and biorhythm disorders; it is also an important antioxidant and hydroxyl radical neutralizer [27]. Day-sleep does not provide this quality and is not as full-fledged as the night sleep taking into account its further malignance to natural biorhythms of a human organism.
Individual daily need for sleep plays an important role in subject shift work tolerance. Subjects with lower need are generally more tolerant to shift work [25]. The rate of tolerance to shift work is inversely proportional to age; in subjects aged 50 and older is the tolerance poor and unacceptable [25].
MATERIALS AND METHODS
Sleep quality in general nurses
Nowadays, the health care providers in the Czech Republic are operating in two-shift work, alternating day and night shifts in partly overlapping (in order to refer patients and documentation) thirteen-hour intervals. This model is more acceptable for employers than the three-shift work previously used work because of its lower organizational and administrative workload during planning, employee register and following salary statement and also pose smaller demands on number of medical personnel [1]. The two-shift work is also preferred by employees because of private life fragmentation decline by extension of the time interval between each shift [6].
The ratio of night shifts grew simultaneously with the introduction of two-shift work which is proved to disturb physiological processes in the organism and lead to increased load of organism in both the psychical and the physical levels [13]. Increased load and fatigue are the main reasons for professional errors [2, 8]. The largest amount of generated errors is made between midnight and 6 am, whilst the most errors are made in delivering medication [25]. Up to double difference in number of errors was recorded between the 8-hour and 12-hour shift [29]. People after night shift sleep on average 2–3 hours less than is their usual sleep need [1, 2, 6].
Research objectives
The research objectives were to investigate the impact of shift work on sleep quality of general nurses and the relation between sleep disorders and anxiety level in general nurses.
Data collection methodology
The quantitative approach was used to carry out the research using a questionnaire investigation with two questionnaires: Pittsburgh Sleep Quality Index (PSQI) and Beck anxiety inventory (BAI). PSQI – Pittsburgh Sleep Quality Index was created in 1988 at the University of Pittsburgh (see link). Currently, the guarantor of the PSQI is an independent Sleep Medicine Institute at the University of Pittsburgh. The Czech version of PSQI was obtained from National Institute of Mental Health, office VP5 – Sleep medicine and chronobio-logy, with the kind permission from Jitka Bušková, M.D., Ph.D. The questionnaire looks at seven components determining sleep quality in various areas, namely subjective perception of sleep quality, sleep latency, duration of sleep, habitual sleep efficiency, sleep disorders, sleeping medication and daytime dysfunction. These components are subsequently scored and their sum provides not only the overall view of a persons’s sleep quality but also diagnostics of possible problem areas on the basis of score gain in particular components. Standardized metrics, which is included in the licensed version of the questionnaire, serves for the evaluating of PSQI. The value obtained of total PSQI index can range from 0 point (absolutely no sleep disorders) to 21 points (serious sleep disorders in all subject components). BAI – Beck Anxiety Inventory was created by Beck and his colleagues and it is used both in its basic form (BAI) and in its subsequent mutations (STAI – State-Trait Anxiety Inventory, BAIT – Beck Anxiety Inventory-Trait). Foreign studies characterise BAI as a very accurate tool for measuring anxiety symptoms [14, 20]. The questionnaire consists of 21 items and looks at the anxiety symptoms over the last week on the Likert scale [22].
Sample
Researched sample of respondents consisted of general nurses working in shifts in departments of orthopaedics, neurology, urology, geriatrics, otho-rhinolaryngology and department of long-term care and aftercare. Research survey was conducted in selected workplaces of three hospitals in the Olomouc region in 2016. The realization agreement was ensured before initialization of the research survey. There were 200 questionnaires distributed (100 questionnaires for the control group and 100 questionnaires for the experimental group). Return rate was 60.5%, which 121 questionnaires. Fifty-six nurses of average age 40.77 (SD = 9.44) and work experience 20.70 years (SD = 10.05) were working one-shift work and sixty-five nurses aged on verage 38.29 (SD = 9.36) and work experience 17.57 years (SD = 8.97) were working in shifts. Data have been processed statistically and evaluated with the aid of statistic software IBM SPSS Statistics 19. Kolmogorov-Smirnov test was used to acquired data scoping normality. Based on scoping of abnormal data distribution, Mann-Whitney test at 5% significance level and Spearman’s rank correlation coefficient at significance levels 5% and 1 % were used for further statistical processing.
RESEARCH RESULTS
In total 121 respondents took part in the research. The control group comprised of general nurses performing one-shift work. All the respondents were women.
PSQI score D (121) = 0.108, p=0.001 as well as BAI score D (121) = 0.146, p=0.000 revealed significant deviation from the normal data distribution. Average duration of sleep in the experimental group was 6.41 hours while the average duration of sleep in the control group was 6.89 hours (Table No.1)
1. Comparison of average sleep duration in experimental and control group 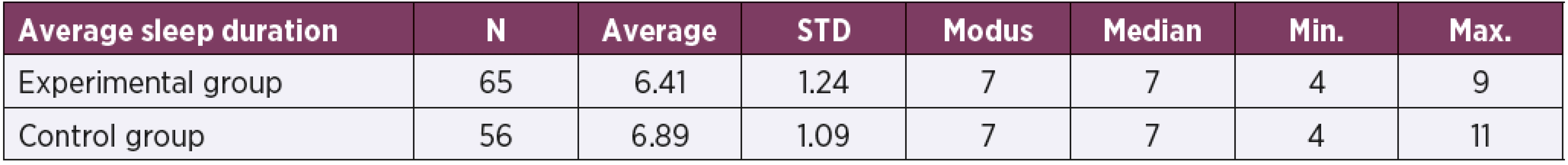
N – Number of respondents, STD – Standard deviation, Min. – minimum, Max. – Maximum The overall rate of sleep disorders in general nurses performing shift work (experimental group) and the overall rate of sleep disorders in general nurses performing only morning-shift work (control group) was ascertained with PSQI questionnaire evaluation. See Table No. 2.
2. Comparison of average global PSQI scores in experimental and control group 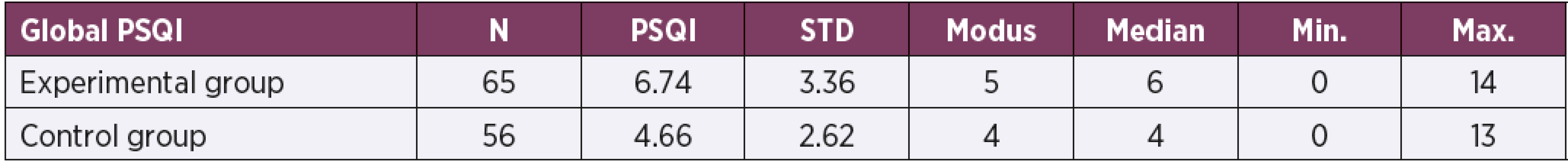
N – Number of respondents, PSQI – average global value of PSQI, STD – Standard deviation, Min. – minimum, Max. – Maximum Mann-Whitney test implied the group of general nurses working in shifts (the experimental group) has a higher ratio of sleep disorders (Mdn = 6) than the control group (Mdn = 4), U = 2.500, p = 0.000, r= -0.323.
The total rate of anxiety in general nurses performing the shift work (experimental group) and the overall rate of sleep disorders in general nur-ses performing only morning-shift work (control group) is shown in Table 3.
3. Comparison of global average BAI in experimental and control groups 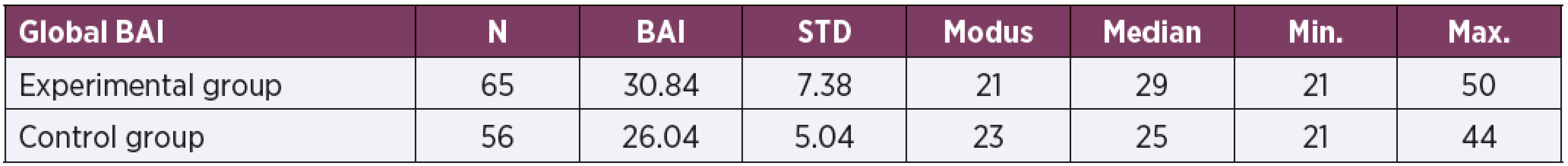
N – Number of respondents, BAI – average global value of Beck anxiety inventory, STD – Standard deviation, Min. – minimum, Max. – Maximum In the experimental group, an average global value of BAI = 30.84 was detected while in the control group there was BAI = 26.04.
Mann-Whitney test implied the group of gene-ral nurses performing shift work has higher ratio of anxiety symptoms (Mdn = 29) than the group of nurses performing one-shift work (Mdn = 25), U = 2.374, p = 0.04, r = -0.262.
Spearman’s rank correlation coefficient confirmed the existence of a relation between anxiety symptoms ratio (BAI) and global sleep disorders symptoms ratio (PSQI) rs = 0.596, p ≤ 0.01. With raising ratio of sleep disorders the anxiety level in general nurses raises as well.
A substantial connection between anxiety symptoms ratio and daytime dysfunction ratio, rs = 0.337, p ≤ 0.01 has been identified. The results are stated in Table 4.
4. Resultant correlations 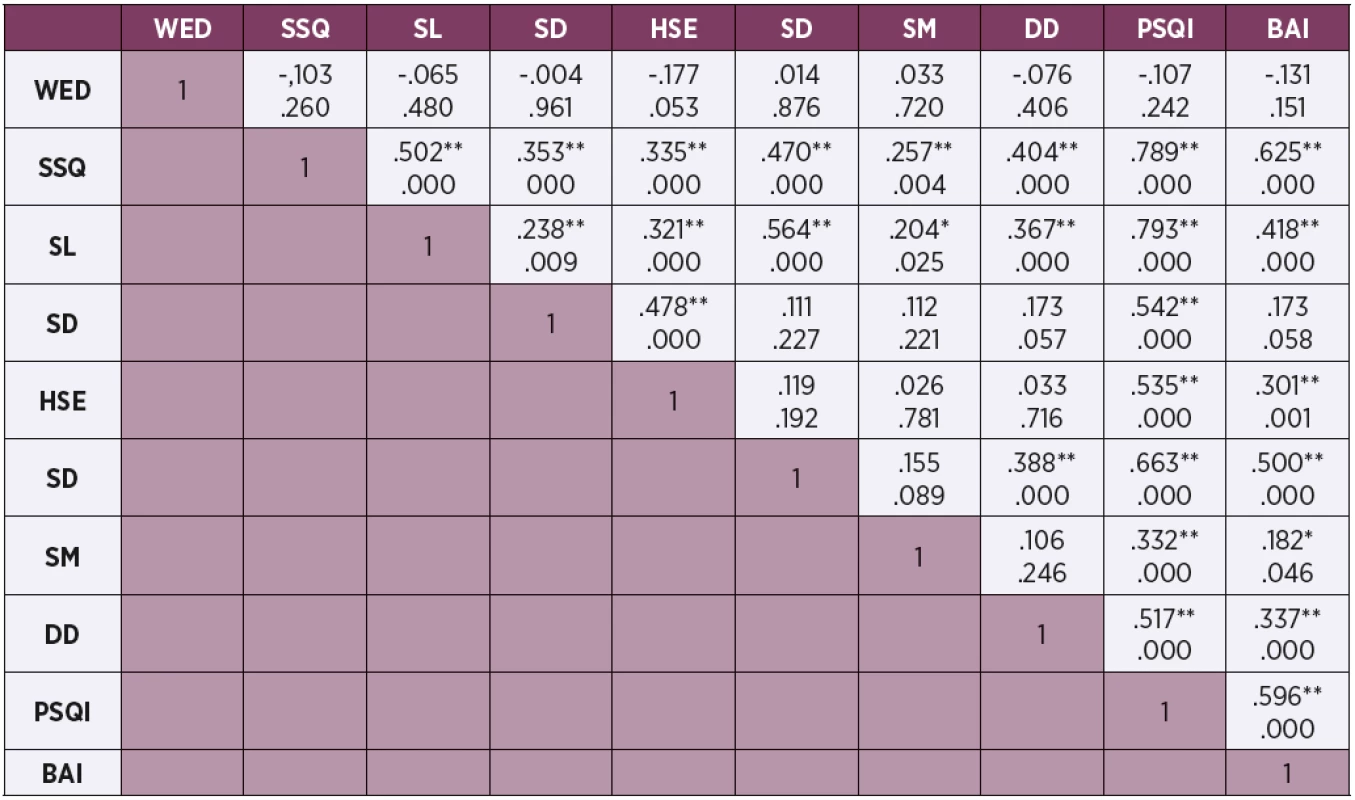
WED – work experience duration, SSQ – subjective sleep quality, SL – sleep latency, SD – sleep duration, HSE – habitual sleep efficiency, SD – sleep disorders, SM – sleeping medications, DD – daytime dysfunction, PSQI – Pittsburgh Sleep Quality Index, BAI – Beck anxiety inventory Spearman’s rank correlation coefficient has not detected a relation among anxiety level, sleep disorders or work experience duration of researched sample of respondents.
DISCUSSION
The aim of this research survey was to explore the impact of shift work on sleep quality and anxiety in general nurses. It was ascertained that average sleep duration in general nurses in shift work is shorter than in nurses working a single-shift which corresponds to the result of Banks and Dingese [2] who discovered that the respondents working morning shifts border on identified average (6.8 hours on workdays and 7.4 hours at the weekends – average value = 6.97 hours), while respondents working in shifts range under the average value of sleep duration, which is on average half an hour daily less. General nurses working in shifts could be designated as a group at risk of sleep deprivation symptoms, i.e. lapses in attention, slowed reactions, short-term errors or impaired ability of data processing, because the negative impact of shift work on sleep disorders ratio in workers was proven regardless of discipline [4, 5, 6, 11, 25].
The results of our research confirm the existence of significant difference in sleep quality between general nurses performing shift work and general nurses performing morning shifts. This finding corresponds to similar research of authors van Mark, Weiler et al [15] who used PSQI questionnaire and also confirmed the difference in sleep quality to the detriment of shift work.
Hrušková et al. was assessing the psychic load in 167 employees in three social welfare facilities. In healthcare professionals, especially in women, there was a significant psychical load at work, frustration symptoms resulting from not only their empathy with patients staying long time out of their families and dying but also from the negatives coming form long-term shift work and often demanded overtime work [12].
Křivohlavý states the necessity of shift work adaptation as one of the key stressor potentially causing anxiety in general nurses [13]. Many stu-dies confirm direct connection between shift work and risk of developing anxiety [7, 9, 11]. The results of our research also confirm significantly higher anxiety level in general nurses doing shift work in comparison to general nurses working morning--shifts only. A research by Ruggiero gave similar results, using Beck anxiety inventory it confirmed a significant relation between shift work and anxiety symptoms level [24]. Average value of BAI index in nurses performing shift work made 25.94 (ave-rage BAI in experimental group revealed in our research = 26.04) and average value of BAI index in nurses engaged only in morning-shift work was 31.05 (average BAI in control group revealed in this work = 30, 84).
Many other studies confirm the mutual relation between sleep disorders ratio and anxiety level [11, 18, 19, 23, 28]. Waghorn et al. particularize the above mentioned with statement that in individuals with some form of anxiety disorder the daytime dysfunction symptoms are expressed very negatively (i.e. uncontrollable urge to sleep, sudden concentration and orientation loss) and pose increased level of error making when performing activities [24].
The results of our research have proved significant relation between sleep disorders level and anxiety level in general nurses. At the same time a significant relation between anxiety level and daytime dysfunction level in experimental group of general nurses has been proven. Similarly, Ruggiero with the aid of PSQI and BAI in nurse performing shifts in emergency department confirmed the existence of relation between anxiety level and sleep disorders level in researched group of nurses [24].
Presented research has not proven the relation between respondents’ length of work experience and sleep disorders level or anxiety level, which corresponds to findings of Dinges and Dongen that negative impacts of sleep deprivation caused by work load are from long-term point of view similar in all subjects with no regard to their individual parameters [6].
The limitation of this pilot research is the low number of survey respondents, respondent sample included only women and it was carried out in three healthcare providers.
CONCLUSION
General nurses working in shifts suffer more from sleep disorders and anxiety symptoms, which influence daytime dysfunctions, in contrast to nurses working in one-shift work. Deterioration of cognitive functions in nurses, their confirmed increase in error making and daytime dysfunctions are negatively reflected in the quality of care provided and affect subjective satisfaction of patients. Consequently, sleep disorders have a direct impact on health care providers. The consequences can be represented in a form of economic and legal risk associated with possible adverse events caused by a nurse influenced by impact of sleep or anxiety disorders.
During shifts planning for nurses, it is vital to maximize the space for sleep deficit compensation caused by insufficient sleep after working a night shift. It is therefore necessary to promote sleep hygiene in nurses and also their biorhythms when possible.
Do redakce došlo dne 17. 10. 2016. Do tisku přijato dne 25. 10. 2016.
Adresa pro korespondenci:
Mgr. Šárka Vévodová, Ph.D.
Ústav společenských a humanitních věd
Hněvotínská 3
775 15 Olomouc
e-mail: sarka.vevodova@upol.cz
Sources
1. Äkerstedt, T. Shift work and disturbed sleep/wakefulness. Occupational Medicine, 2003, 53, 2, p. 89–94 [cit. 2016-05-04]. doi: 10.1093/occmed/kqg046. Available from: http://occmed.oxfordjournals.org/content/53/2/89.full.pdf+html.
2. Banks, S., Dinges, D. Behavioral and Physiological Consequences of Sleep Restriction. Journal of Clinical Sleep Medicine, 2007, 5, 3, p. 519-528 [cit. 2016-05-04]. Available from: http://www.med.upenn.edu/uep/user_documents/Banks2007-Behavioralandphysiologicalconsequencesofsleeprestrictioninhumans.pdf.
3. Bartošíková, I. O syndromu vyhoření pro zdravotní sestry. Brno: Národní centrum ošetřovatelství a nelékařských zdravotnických oborů, 2006, 86 p.
4. Borzová, C. Nespavost a jiné poruchy spánku: pro nelékařské zdravotnické obory. Praha: Grada, 2009, 144 p.
5. Buysse, D., J., Monk, T., H., Carrier, J., Begley, A. Circadian patterns of sleep, sleepiness, and performance in older and younger adults. Sleep, 2005, 28, 11, p. 1365–1376.
6. Dongen van, H., P., Dinges, D., F. Sleep, circadian rhythms, and psychomotor vigilance. Clin. Sports Med., 2005, 24, 2, p. 237–249, vii-viii. doi:10.1016/j.csm.2004.12.007.
7. Eldevik, M. F., Flo, E., Moen, B. E., Pallesen, S., Bjorvatn, B. Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PloS one, 2013, 8, 8. doi:10.1371/journal.pone.0070882.
8. Ely, J., W., Kaldjian, L., C., D’Alessandro, D., M. Diagnostic errors in primary care: lessons learned. J. Am. Board Fam. Med., 2012, 25, 1, p. 87–97. doi:10.3122/jabfm.2012.01.110174.
9. Flo, E., Pallesen, S., Mageroy, N., Moen, B. E., Gronli, J., Hilde Nordhus, I., Bjorvatn, B. Shift work disorder in nurses – assessment, prevalence and related health problems, PLoS One, 2012, 7, 4, e33981. doi:10.1371/journal.pone.0033981.
10. Haus, E. Chronobiology in the endocrine system. Advanced Drug Delivery Reviews, 2007, 59, 9–10, p. 985–1014.
11. Hegney, D. G., Craigie, M., Hemsworth, D., Osseiran-Moisson, R., Aoun, S., Francis, K., Drury, V. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: study 1 results. J. Nurs. Manag., 2014, 22, 4, p. 506–518.
12. Hrušková, M., Strýčková, M., Buchancová, J., Cigániková, Z. Hodnotenie psychickej pracovnej záťaže u profesií v domovoch sociálnej starostlivosti, v nemocnično-poliklinickom zariadení a vo vybraných nezdravotníckych oblastiach. Pracov. Lék., 2012, 64, 4, p. 147–155.
13. Křivohlavý, J. Sestra a stres: Příručka pro duševní pohodu. Praha: Grada, 2010, 128 s.
14. Leyfer, O. T., Ruberg, L. J., Woodruff-Borden. J. Examination of the utility of the Beck Anxiety Inventory and its factors as a screener for anxiety disorders. Journal of Anxiety Disorders, 2006, 20, 4, p. 444–458. doi: 10.1016/j.janxdis.2005.05.004.
15. Mark van, A., Weiler, S. W., Schroder, M., Otto, A., Jauch-Chara, K., Groneberg, D. A., Spallek, M., Kasse R., Kalsdorf, B. The impact of shift work induced chronic circadian disruption on IL-6 and TNF-alpha immune responses. J. Occup. Med. Toxicol., 2010, 5, 18. doi:10.1186/1745-6673-5-18.
16. Marx, D. Akreditační standardy – jedna z cest k minimalizaci chyb. Zdravotnické noviny, 2001, 11, 9, p. 22.
17. Moorcroft, W., H. Understanding sleep and dreaming. Boston: Springer, 2013, 369 p.
18. Nevšímalová, S., Šonka, K. et al. Poruchy spánku a bdění. Praha: Galén, 2007, 345 s.
19. Ohayon, M. M., Roth, T. Place of chronic insomnia in the course of depressive and anxiety disorders. Journal of Psychiatric Research, 2003, 37, 1, p. 9–15. doi: 10.1016/S0022-3956(02)00052-3.
20. Osman, A., Hoffman, J., Barrios, F. X., Kopper, B. A., Breitenstein, J. L., Hahn, S. K. Factor structure, reliability, and validity of the Beck Anxiety Inventory in adolescent psychiatric inpatients. J. Clin. Psychol., 2002, 58, 4, p. 443–456. doi: 10.1002/jclp.1154.
21. Plháková, A. Spánek a snění: vědecké poznatky a jejich psychoterapeutické využití. Praha: Portál, 2013, 258 s.
22. Praško, J., Espa-Červená, K., Závěšická, L. Nespavost: zvládání nespavosti. Praha: Portál, 2004, 102 s.
23. Rogers, A. E. The Effects of Fatigue and Sleepiness on Nurse Performance and Patient Safety. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD) [online]. 2008. [cit. 2016-05-04]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK2645/.
24. Ruggiero, J., S. Correlates of fatigue in critical care nurses.Research in Nursing & Health, 2003, 26, 6, p. 434–444. doi:10.1002/nur.10106.
25. Scott, L. D., Hwang, W. T., Rogers, A. E., Nysse, T., Dean, G. E.,Dinges, D. F. The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep, 2007, 30, 12, p. 1801–1807.
26. Šonka, K., Fiksa, J., Horváth, E., Kemlink, D., Süssova, J., Böhm, J., Šebesta, V., Volná, J., Nevšímalová, S. Sleep and fasciculations in amyotrophic lateral sclerosis. Somnologie - Schlafforschung und Schlafmedizin, 2004, 8, 1, p. 25–30. doi:10.1111/j.1439-054X.2003.00010.x.
27. Tuček, M., Cikrt, M., Pelclová, D. Pracovní lékařství pro praxi. Praha: Grada Publishing, a. s., 2005, 327 s.
28. Waghorn, G., Chant, D., White, P., Whiteford, H. Disability, employment and work performance among people with ICD-10 anxiety disorders. Aust. N. Z. J. Psychiatry, 2005, 39, 1–2, p. 55–66. doi:10.1111/j.1440-1614.2005.01510.x.
29. Wagstaff, A., S., Sigstad Lie, J., A. Shift and night work and long working hours – a systematic review of safety implications. Scand. J. Work Environ. Health, 2011, 37, 3, p. 173–185. doi:10.5271/sjweh.3146.
30. Weyerer, S., Dilling, H. Prevalence and treatment of insomnia in the community: results from the Upper Bavarian Field Study. Sleep, 1991, 14, 5, p. 392–398.
Labels
Hygiene and epidemiology Hyperbaric medicine Occupational medicine
Article was published inOccupational Medicine

2016 Issue 3-
All articles in this issue
- Analysis of subjective assessment of thermal-humidity microclimatic conditions in selected production organizations
- Auto-kinesio-therapy in the carpal tunnel syndrome
- Providing brief interventions and smoking prevalencein employees of the Královské Vinohrady Teaching Hospital and Third Faculty of Medicine of Charles Universityin Prague
- The carpal tunnel syndrome as viewed by the general practitioner – case report
- Leptospirosis with a rare combination of complications
- The impact of shift work on sleep and anxiety in general nurses
- Occupational Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- The carpal tunnel syndrome as viewed by the general practitioner – case report
- The impact of shift work on sleep and anxiety in general nurses
- Auto-kinesio-therapy in the carpal tunnel syndrome
- Leptospirosis with a rare combination of complications
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

