-
Medical journals
- Career
HAS A GLOMUS TUMOR ALWAYS A QUICK DIAGNOSIS?
Authors: J. Pilný 1,2,4; A. Švarc 3; H. Vodová 4,5; J. Kletenský 6; P. Tichá 6; A. Sukop 6
Authors‘ workplace: Orthopaedics Department, Hospital Nové Město na Moravě, Czech Republic 1; Faculty of Health Studies, Pardubice University, Czech Republic 2; Universitaetklinik für Unfallchirurgie Innsbruck, Austria 3; Department of Anatomy, Medical Faculty, Charles University, Hradec Králové, Czech Republic 4; Orthopaedics Department, Hospital Rychnov nad Kněžnou, Czech Republic 5; Department of Plastic Surgery, Third Faculty of Medicine, Charles University, and Kralovské Vinohrady Teaching Hospital, Prague, Czech Republic 6
Published in: ACTA CHIRURGIAE PLASTICAE, 59, 2, 2017, pp. 82-84
INTRODUCTION
A glomus tumour is a rare and benign vascular tumour. The normal glomus is a neuromyoarterial body. It was first described in 1821 by Wood, but histologically was glomus tumor described in 1924 by Masson.1 It occurs mostly under the fingernails and very rarely in other locations. They constitute less than 2% of soft tissue tumors of the hand (0.2% of soft tissue tumors of the human body).2 Quite exceptionally, the glomus tumor can present in multiple forms. Clinically it manifests as a reaction to cold with sharp resting pain, which increases during nail palpation or when the locus is tapped.
During an examination, the glomus tumor under the nail may not be visible or it may present as a bluish discoloration localized over the tumor.
Typical signs and symptoms (pain, tenderness and temperature sensitivity), obvious during the clinical examination, along with patient history, are usually clear enough for the diagnosis. Ultrasound diagnostics is not used in our conditions because we do not have special probes available. Currently, the gold standard for visualization and diagnosis of the tumor is magnetic resonance imaging (MRI), which is suitable for planning surgical management. (Fig. 1) Although specific symptoms for this disease are quite clear, there is still a delay between the time of onset of the symptoms to diagnosis and appropriate surgical therapy. The authors follow the time from the beginning of the symptoms until the diagnosis and then until treatment of the problem.
1. MRI of glomus tumor (a sagittal view) 
MATERIAL AND METHODS
The Outpatient Orthopaedic Department of the Hospital in Pardubice focused on hand surgery between the years 2004–2012. Totally 5 patients were diagnosed with glomus tumors of the distal phalanges of the hand. It concerned 3 women and 2 men, with an average age of 32.2 years (26–47 years). During the first examination, we monitored the duration of symptoms, number and speciality of the doctors who examined the patient and subsequent diagnostic procedures. All patients were clinically examined – monitored for the nail bed changes and a test was performed by immersion in cold water. When the cold test was positive, all patients underwent MRI that showed presence of a focus under the nail. The patients were indicated for surgical revision under local anaesthesia (4 patients) and one patient wished the procedure to be performed under general anaesthesia. The operation was performed in a bloodless field with the usage of magnifying loupes; the nail was released proximo-distally and after extirpation of the tumor was the nail bed closed with absorbable sutures. (Fig. 2, 3) For all surgery, the magnification was noticeable by attenuation of the soft tissues over the tumor. The tissue specimens in all patients were histologically verified. The patients were followed up for 2 years. At the first examination, we monitored how long the patient’s discomfort lasted, how long the patients were examined and what examinations they underwent.
2. Nail bed after removal of the glomus tumor 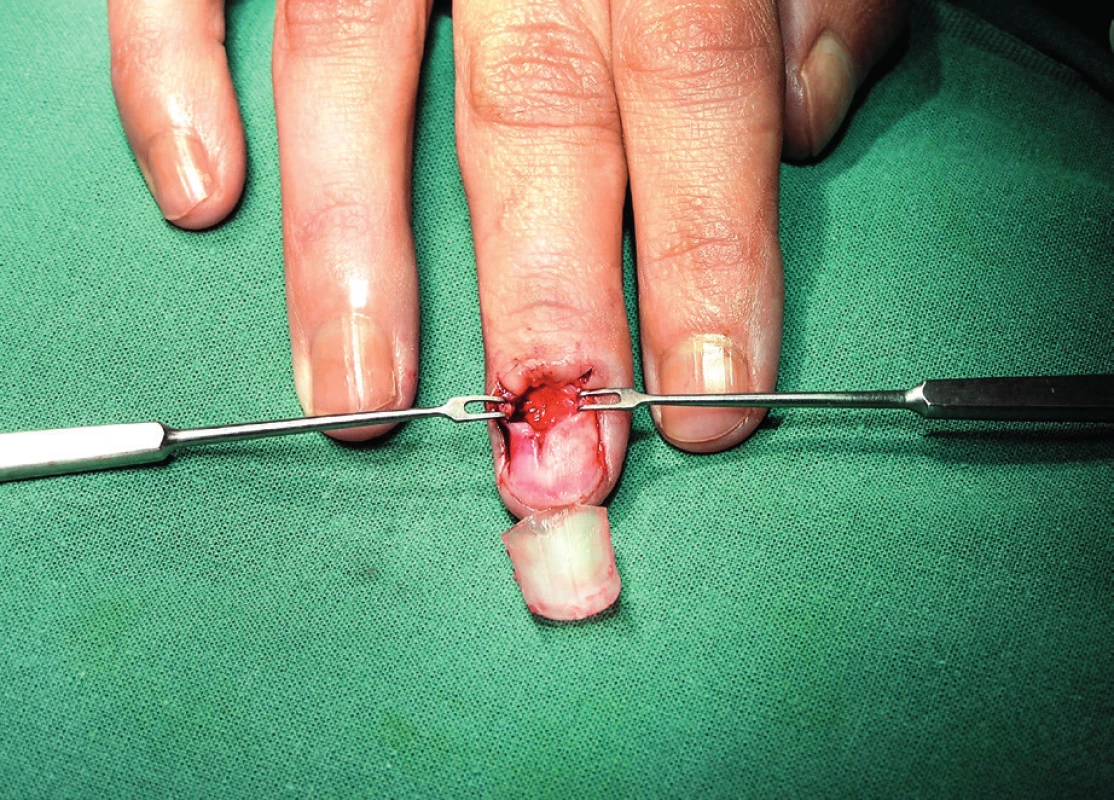
RESULTS
During the primary examination, it was found that patients suffered from clinical symptoms for an average of 2.4 years (0.5 years–6 years). In our group, each patient was examined by an average of 5.4 physicians (3–9 physicians). Speciality of the doctors by whom the patients were examined is shown in the Chart 1. The chart does not include general practitioners. The patient was sometimes examined by several doctors in case of one medical specialty. On examination before surgery, there were changes of the nail bed recorded in three cases and two patients showed no changes.
Chart 1. Physician’s expertise and the number of patients who were examined 
During the follow up of the patients for 2 years post-op, relapse occurred only in one case with the need for reoperation. After the reoperation, no complications or other relapse occurred. During the follow up 2 years after surgery, 4 patients were without nail deformity. Only one patient had a deformity of the nail. In this case, the tumor covered nearly the entire nail bed and as a consequence it could not be reconstructed. Numbness of the distal phalanx was not recorded.
DISCUSSION
Because the glomus tumor is a rare lesion, occurring most frequently in the nail bed, its early diagnosis is still a problem. The patient is often referred to many specialists, who only exclude the cause by its physical appearance and from the point of view of their specialty.
Each patient was examined by an average of 5.4 doctors and the diagnosis was made after 2.4 years. In the literature, we often encounter a similar time frame from the onset of symptoms until proper diagnosis. Hamdi (2011) states the time of diagnosis 1.9 years and Assmus (2002) 8 years. Both authors report delays due to inaccurate diagnosis when patients were treated for different diseases.
Another widely discussed issue is what approach to use3,4. In case of the approach through the nail or its deflection, nail deformity is often described5. The same author also describes changes in the sensitivity of the nail and the distal phalanx6. To prevent nail deformity, Vasisht (2004) published the treatment of glomus tumor using the lateral subperiosteal approach as described by Garg (2016).7,8 Lateral subperiosteal approach, where the authors prefer the lateral side after loosening of the nail side from the lateral tumor. Its advantage is seen in prevention of nail bed deformation. Both authors agree on the necessity for accurate preoperative diagnosis using magnetic resonance imaging of the location and the lesion to determine accurate access point. We believe that magnetic resonance imaging is not necessary if clinical symptoms are obvious and changes of the nail bed under the nail are obvious. If the clinical examination was positive but the tumor localization was not clear, we will perform magnetic resonance imaging to confirm the finding and to determine the size of the lesion. We did not indicate ultrasound examination because, after consultation with the radiologists, it was found that suitable equipment was not available.
In our department, postoperative deformity of the nail was recorded in only one case did not attribute to incomplete survival of the nail bed after the extirpation of the tumor. Relapse occurred in one case; it was our first patient, in whom the tumor was not completely excised. The reason was that the surgeon was worried about the safe treatment of the nail bed. For this reason, the tumor was not completely removed. The occurrence of multilocular forms, have not been encountered in our department, because these forms are very rare.
CONCLUSION
Although the clinical signs and symptoms of the glomus tumors are very obvious, there is still a long diagnostic period. It would certainly be ideal for patients with any persistent hand symptoms to be referred to a department, which specializes in hand surgery, where the diagnosis will be established faster, more effectively and which would be far more beneficial from the economic point of view.
Statement: The authors declare that their work and documents are original and concurrently agree with publication.
Corresponding author:
Assoc. Prof. Jaroslav Pilný, M.D., Ph.D.
Orthopaedics Department
Hospital Nové Město na Moravě
Žďárská 610, 592 31 Nové Město na Moravě
Czech Republic
E-mail: pilny@ortopedie-traumatologie.cz
Sources
1. Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med. 2008 Sep;132(9):1448–52.
2. International Agency for Research on Cancer. Pathology and Genetics of Tumours of Soft Tissue and Bone. 2002; St. Louis: WHO Press: 136–7.
3. Hamdi MF. Glomus tumour of fingertip: report of eight cases and literature review. Musculoskelet Surg. 2011 Dec; 95(3):237–40.
4. Assmus H, Dombert T. Glomus tumours of the extremities: localisation and operative treatment in 36 cases. Handchir Mikrochir Plast Chir. 2002 Mar;34(2):103–7.
5. Lee W, Kwon SB, Cho SH, Eo SR, Kwon C. Glomus tumor of the hand. Arch Plast Surg. 2015 May; 42(3):295–301.
6. Lee SH, Roh MR, Chung KY. Subungual glomus tumors: surgical approach and outcome based on tumor location. Dermatol Surg. 2013 Jul; 39(7):1017–22.
7. Vasisht B, Watson HK, Joseph E, Lionelli GT. Digital glomus tumors: a 29-year experience with a lateral subperiosteal approach. Plast Reconstr Surg. 2004 Nov; 114(6):1486–9.
8. Garg B, Machhindra MV, Tiwari V, Shankar V, Kotwal P. Nail-preserving modified lateral subperiosteal approach for subungual glomus tumour: a novel surgical approach. Musculoskelet Surg. 2016 Apr;100(1):43–8.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2017 Issue 2-
All articles in this issue
- Editorial
- COMPLICATIONS OF LOWER EXTREMITY HEMATOMAS IN PATIENTS WITH PRE-INJURY WARFARINE USE
- SURGICAL CORRECTION OF LABIA MINORA HYPERTROPHY, A PERSONAL TECHNIQUE
- SUTURE VERSUS FIBRIN GLUE MICRONEURAL ANASTOMOSIS OF THE FEMORAL NERVE IN SPRAGUE DEWLY RAT MODEL. A COMPARATIVE EXPERIMENTAL ASSESSMENT OF THE CLINICAL, HISTOLOGICAL AND STATISTICAL FEATURES
- INTRAOPERATIVE FAT GRAFTING INTO THE PECTORALIS AND LATISSIMUS DORSI MUSCLES-NOVEL MODIFICATION OF AUTOLOGOUS BREAST RECONSTRUCTION WITH EXTENDED LATISSIMUS DORSI FLAP
- HAS A GLOMUS TUMOR ALWAYS A QUICK DIAGNOSIS?
- CURRENT CONCEPTS IN PERIPHERAL NERVE INJURY REPAIR
- SUBACUTE ARTERIAL BLEEDING AFTER SIMULTANEOUS MASTOPEXY AND BREAST AUGMENTATION WITH IMPLANTS: CASE REPORT
- AUTOLOGOUS FAT TRANSFER, BREAST LIPOMODELLING AND FAT TRANSFER TO THE FACE: CURRENT GOLD STANDARDS AND EMERGING NEW DATA
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- SURGICAL CORRECTION OF LABIA MINORA HYPERTROPHY, A PERSONAL TECHNIQUE
- INTRAOPERATIVE FAT GRAFTING INTO THE PECTORALIS AND LATISSIMUS DORSI MUSCLES-NOVEL MODIFICATION OF AUTOLOGOUS BREAST RECONSTRUCTION WITH EXTENDED LATISSIMUS DORSI FLAP
- COMPLICATIONS OF LOWER EXTREMITY HEMATOMAS IN PATIENTS WITH PRE-INJURY WARFARINE USE
- HAS A GLOMUS TUMOR ALWAYS A QUICK DIAGNOSIS?
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


